Pancreas
– – Cancer of the pancreas : Definition
Definition
The cancer of the pancreas starts in fabrics of your pancreas.
The pancreas is a body located behind the stomach, in the upper part and major of the abdomen (left retro péritonéale).
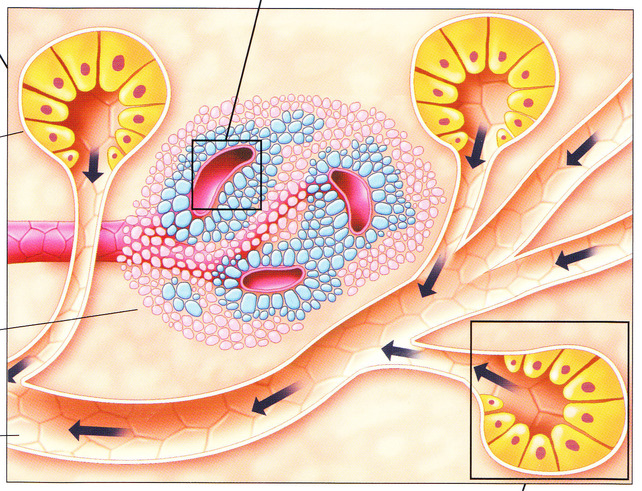
The pancreas is part of the digestive system and endocrinal, ace
It secretes enzymes which facilitate digestion and of the hormones which help to control the metabolism of sugars
The pancreatic liquid of secretion composes of digestive bicarbonate and enzymes: amylase, lipase, protease are transferred along a conduit located in its center the pancreatic channel of Wirsung
That it is connected to the cholédoque channel, which comes from the liver while transporting the bile
Once the food left the stomach, pancreatic juices and the bile help to continue their digestion in the duodenum
The pancreas also is part of the endocrinal device
It secretes insulin as well as glucagon and other hormones which return in the blood circulation to help the organization to use and store energy coming from food.
- The cancer of the pancreas generally occurs at people of more than 65 years
The cancer of the pancreas is propagated generally quickly. - It is seldom detected at the beginning what is the main reason for which often surgical ablation is not possible.
- The cancer of the pancreas is often of bad forecast, even when he is diagnosed early
The cancer of the pancreas occurs when a pancreatic cell develops genetic mutations.
These changes cause the growth and cellular proliferation uncontrolled with the formation of a tumour
The type of cells implied in a cancer of the pancreas can help to determine the best treatment
Type of pancreatic cancer
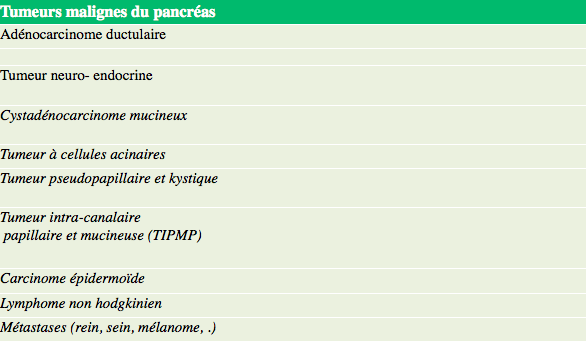
The cancer of the pancreas appears in the conduits transporting the pancreatic gastric juices.
The majority of cancers of the pancreas are adenocarcinomists (canal adenocarcinomist excrèto pancreas)
It is rare that the cancer of the pancreas occurs in the endocrine cells which manufacture the hormones.
Most frequent cancers neuro endocrine of the pancreas are the nonfunctional insulinomists, gastrinomists and tumours
– – Pancreas : Causes and risk factors
The factors which can increase the risk to develop a cancer of the pancreas are the following
- Risk factors
- age > 60 years
- tobacco addiction
- obesity
- mode rich in greases and animal proteins (nitrates used to preserve the meat)
- pancréatite chronic
- personal or family antecedents of cancer of the pancreas
- Hereditary disorders genetics such as: syndrome of Lynch or hereditary cancer colorectal without polypose (HNPCC)
- Syndrome of Peutz-Jeghers change of gene BRCA2 (hereditary cancer of the centre and the ovary)
The cancer of the pancreas can sometimes develop in the absence of all these risk factors.
– – Signs and symptoms of the cancer of the pancreas
Symptoms
The cancer of the pancreas is often asymptomatic
A cancer of the pancreas can proliferate until reaching a relatively large size without causing symptoms, owing to the fact that the pancreas is
deprived of nervous terminations able to send signals of pain to the brain
When the tumour reaches a certain dimension or starts to extend beyond the pancreas, it can cause symptoms:
- symptoms
- Pain Frequency: 60 80%. The pain is localised in the area of the stomach and can be irradiated in the back
- Ictère jaundice Frequency the 40-80% skin and the white of the eyes take a yellow color, the urine becomes darker because the tumour blocks the cholédoque channel and the passage of the bile
- Prurit Frequency 25% Prurit (itched one) is associated with the ictère
- Slimming Frequency 50 80% The weight loss is often unexplained, massive and fast
- Nauseas Frequency 50%
Consult your attending physician if you feel an unexplained weight loss, abdominal pains, a ictère.
Health problems other than cancer can cause similar signs and symptoms.
After having checked your medical antecedents and to have examined to you, your doctor can address to you to the surgical consultation if he will suspect the presence of a cancer of the pancreas.
– – The cancer of the pancreas : diagnostic
Diagnosis
To diagnose the cancer of the pancreas
If your doctor suspects a cancer of the pancreas, the realization of several complementary examinations will prescribe you; the objective being first of all to make diagnoses it tumour and then to see whether cancer were propagated (stadification)
The stadification makes it possible to say if it is possible to withdraw the lesion by surgical way.
Biological analyses
Starting from samples of your blood, one controls your bodies up to what point function normally.
One checks the signs and the biological importance of possible a ictère (increase bilirubine, alkaline phosphatase, etc)
It is programmed the blood proportioning of certain substances (markers) which can be detected in the blood of the people reached of cancer.
The two tumoral markers proportioned in the cases of cancer of the pancreas are the proteins CA19-9 and ACE
The control of marker CA19-9 is most reliable: it is mainly used to check the individual reaction to the selected treatment of the cancer of the pancreas.
Techniques of imagery?
These techniques make it possible examine a closer examination of fabrics, bodies and bones.
Echography uses high frequency sound waves to create animated images of the internal bodies, including the blister, the bile duct and the pancreas.
The CT scanner or TDM and magnetic resonance MRI are different techniques used with an aim of obtaining an image of the tumour and of checking if it extended.
The MRI uses a powerful magnetic field and radio waves while to scan it (TDM) uses X-rays to visualize your internal bodies
These tests are generally without pain and do not require any anaesthesia.
In certain cases, you can receive an injection of dye (average of iodized contrast, gadolinium) in a vein of your arm to help to highlight the zones of your radiologist wants to see.
Endoscopy
The endoscopy makes it possible to the doctor to examine the interior of certain parts of the body by means of an endoscope.
It is about a narrow and flexible tube, provided with a light and a tiny camera at its end.
The diagnosis of the cancer of the pancreas could require one of the following endoscopic interventions:
ERCP (or CPRE Cholangio – Retrograde Pancréatographie Endoscopic)
A thin and flexible tube, the endoscope, is introduced by the throat to go down to the stomach and to the duodenum and finally to reach the opening of the pancreatic channel (papilla).
The gastroenterologist can then inject by the endoscope a product of contrast and carry out radiographic stereotypes. He locates on radiography any anomaly or blocking of the bile ducts and pancreatic
If the tumour blocks the bile ducts or the duodenum, the gastroenterologist will be able, using the endoscope, to install a small metal tube (called endoprothèse or stent) in order to release the opening
This intervention will require a general anaesthesia.
ECHOENDOSCOPIE or scans endoscopic
The probe of echography (device with ultrasounds) passed through an endoscope in the stomach in order to obtain the images.
This examination also makes it possible to take a sample of cells tumoral (biopsy by echo endoscopy) to have the histological proof of the tumour
Biopsy of the pancreas
A biopsy is generally necessary to establish with certainty a diagnosis of cancer.
This procedure consists in taking a small fabric sample of the pancreas, for examination under the microscope
There exist several methods to carry out a biopsy of the pancreas:
The Biopsy can be carried out by puncture with the fine needle by using the echograph or scan it to direct the needle towards the suspect pancreatic lesion.
The taking away can be done at the time of a CPRE or of a echoendoscopy.
– – Stadification of the cancer of the pancreas
Stadification of the cancer of the pancreas
Once the diagnosis of the cancer of the pancreas is confirmed, It is necessary to determine the stage of cancer.
The stadification of pancreatic cancer consists in defining the size of the tumour and checking if it developed beyond the pancreas, body where it occurred.
Four stages were defined for the cancer of the pancreas.
- Stadiation
- Stage I: Cancer is localised exclusively with the pancreas. The tumour can be of variable size, but it was not propagated with the lymphatic ganglia nor with another part of the body. Stage T1 = size <2cm
T2= cuts > 2cm
NO - Stage II: Cancer was propagated beyond pancreas (T3) with neighbouring fabrics and bodies, but remains surgically résécable
The lymphatic ganglia can be invaded Stage II WITH = T3, N0, M0 B= T1-3, N1, M0 - Stage III: Cancer locally is not résécable.
Cancer was propagated with the principal blood-vessels (mesenteric artery or cœliaque trunk), and sometimes with the lymphatic ganglia located in the vicinity
Stage III
T4, any NR, M0 - Stage IV: Cancer gained other parts of the body such as the liver, the lungs or the abdominal cavity. Stage IV M+
Presence of metastases
It is important to know the stage of cancer: we will help to choose the treatment which is appropriate to you best.
– – Surgical treatment of the cancer of pancreas
Cancer treatment of the pancreas
Surgery
- The decision to resort to the surgery will depend on the size of the tumour and the place where it is.
- One should not operate the patients whose tumour is not résécable or who will not benefit from the resection (stage III and IV)
- During the intervention, one will carry out the total ablation of the tumour and certain surrounding healthy fabrics.
- The intervention will be practised under general anaesthesia (you will be deadened) and you will be hospitalized during several days after the operation.
- The surgical treatment of the cancer of the pancreas is a major intervention, which involves important side-effects and which requires several weeks of convalescence.
- It is important to weigh up well the advantages and possible risks of such an intervention with your surgeon and to take the opinion of your attending physician.
The surgery can make it possible to withdraw entirely the tumour of the pancreas (complete resection RO)
Three types of intervention are possible for a cancer of the not very advanced pancreas.
The DPC, duodeno-pancreatectomy or operation of Whipple
This kind of intervention is practised when the tumour is in the broadest part of the pancreas (the “head”).
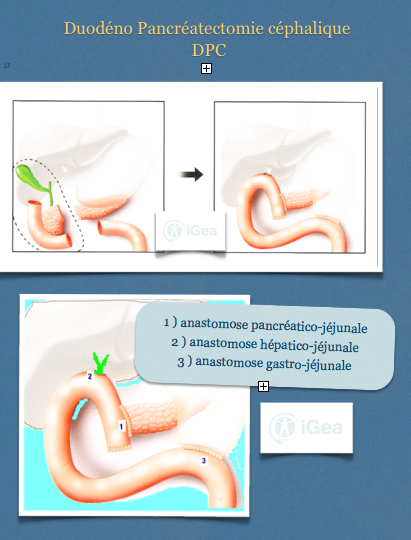
The surgeon withdraws
- the head of the pancreas
- part of the stomach and the duodenum
- the cholédoque channel etla gall bladder
- ganglia lymphatic
Digestive, biliary and pancreatic continuity is restored with 3 joinings (anastomoses)
The DPC comprises an important morbidity.
This morbidity is related to the risk of
- dent or infection (releasing of the pancreatic joining – digestive)
- operational haemorrhage post
- There exists a risk of postoperative mortality related to the complications
A jejunostomy with installation of a probe of food in your intestine can be carried out on a case-by-case basis for better you
to feed. Several days can be passed before you are able to start again to drink and eat correctly
Nauseas and the vomiting can occur if the stomach has difficulty emptying (delay of gastric draining).
After the surgery, convalescence is long.
You will pass 10-15 days or more to the hospital, then to recover during several weeks at the house.
- For ablation partial or total of your pancreas, it will be necessary that you take tablets in order to replace the enzymes which were manufactured before by your pancreas.
- It is possible also that following duodeno-pancreatectomy (DPC) you became diabetic.
The diabetes will be control with drugs or injections of insulin.
You will have to follow this substitution therapy for the rest of your days
Distal Pancreatectomy
One will choose this technique when the tumour is present in other area of the pancreas. The surgeon takes the tail of the pancreas which is
touched, as well as the failure.
This intervention month attends because the cancer of the pancreas distal is often diagnostic late
Total Pancreatectomy
This form of intervention will be selected if cancer is present in the whole of the pancreas.
The surgeon then removes all the pancreas, part of the stomach, the duodenum, the cholédoque channel, the gall bladder, it missed and the ganglia,
lymphatic neighbors.
You become diabetic after total pancreatectomy
This intervention is not very frequent.
Palliative surgery: biliary and gastric derivation
The surgery will make it possible in this case to relieve the symptoms caused by the cancer diagnosed in advanced stage (III – IV) when it cannot be entirely removed.
biliary derivation connecting the cholédoque one to the small intestine so as to allow the passage of the bile and to mitigate the symptom of the ictère
digestive derivation connecting the stomach to the small intestine, so as to circumvent the blocking of the duodenum and to allow an oral food
– – Chemotherapy
Chemotherapy can be part of the treatment for the cancer of the pancreas after a surgical operation.
It will be able to also help to relieve the pain or to attenuate the symptoms if the tumour cannot be removed.
Chemotherapy can be managed in the form of compressed or by injection.
Chemotherapy prevented the development and the propagation of the cancer cells, but it damages also the cells which are in health.
The healthy cells will be able to be restored with time, perhaps but in the interval, the treatment will cause on your premise certain side-effects such as: nauseas, vomiting, loss of appetite, tiredness, loss of hair and increasing risk of infection.
– – Radiotherapy
One can use the radiotherapy, only or in partnership with chemotherapy, to continue the treatment of the cancer of the pancreas instead of the surgery or after the surgery (in auxiliary situation).
It can also help to relieve the pain or to attenuate the symptoms if the tumour cannot be removed.
The radiotherapy make use of a large device which gives the possibility of directing a beam of rays towards the precise place of the tumour.
The radiation damages all the cells, the cancerous ones and also the normals, which are in the trajectory of the beam
– – Prognostic
Forecast cancer of the pancreas
Only less than 5% of the whole of the patients are alive 5 years after the diagnosis of adenocarcinomist of the head of the pancreas.
Among the operated patients “with curative aiming” (complete resection RO), the rate of survival at 5 years is from 10 to 30%.
The result is of as much better than the tumour is smaller and than there is no histological ganglionic invasion (stage I or II A)
Among the patients whose tumour is not résécable, 50% are still alive 6 months after the diagnosis.


Commentaires récents