Valutazione rischio-beneficio della chirurgia bariatrica/per la perdita di peso

Indicazioni e controindicazioni per la chirurgia bariatrica/per la perdita di peso
Nonostante i progressi tecnici nelle pratiche chirurgiche e nell’anestesia, qualsiasi intervento chirurgico effettuato su pazienti gravemente obesi è considerato ad alto rischio.
Per evitare che i rischi del trattamento siano superiori a quelli posti dal problema medico stesso, sono state adottate indicazioni chirurgiche molto specifiche da numerose conferenze di consenso.
La chirurgia è raccomandata per i pazienti il cui IMC (indice di massa corporea) è maggiore o uguale a 40 Kg/m².
Può anche essere raccomandata per persone con un IMC maggiore di 35 Kg/m² che soffrono di una o più patologie concomitanti legate all’obesità (Comorbidità – una malattia o condizione medica presente simultaneamente con un’altra o altre in un paziente).
Inoltre, devono aver avuto un problema di obesità per almeno cinque anni, il trattamento dietetico/conservativo non ha avuto successo e, naturalmente, non devono esserci controindicazioni chirurgiche.
Le controindicazioni chirurgiche includono:
- Dipendenza da sostanze
- Psicosi
- Grave insufficienza epatica o renale (eccetto come parte della preparazione pre-trapianto)
- Malattia infiammatoria intestinale
- Malattie tumorali non controllate
- Storia recente di trombosi o embolia polmonare
Ridurre i rischi pre-operatori:
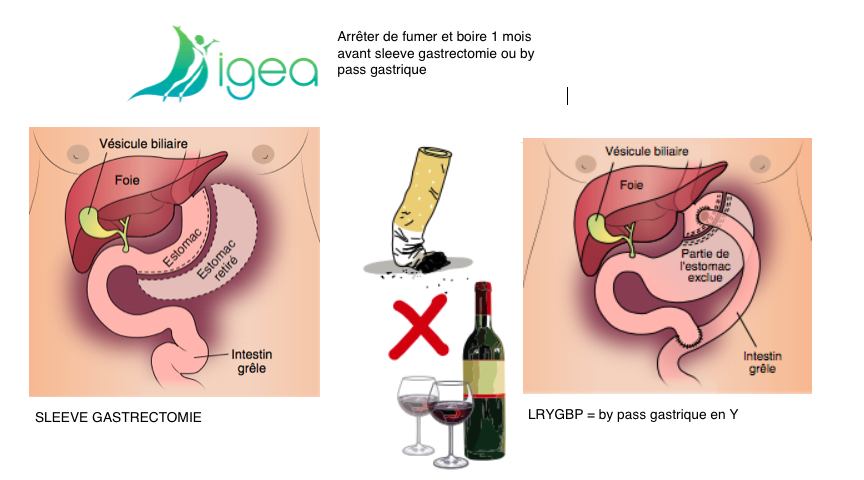
- Smettere di fumare 1 mese prima dell’intervento programmato per ridurre il rischio di complicanze.
- Smettere di bere alcolici 1 mese prima dell’intervento programmato.
- Dieta ipocalorica, povera di zuccheri = riduce la dimensione del fegato. È molto importante iniziare questa dieta 6 settimane prima dell’intervento programmato per garantire un esito positivo.
L’importanza del follow-up chirurgico a vita: l’obesità come malattia cronica
Il rimborso delle spese chirurgiche per l’obesità da parte della tua assicurazione sanitaria è disponibile solo per i pazienti che soddisfano questi criteri di selezione.
Tutti i fascicoli dei pazienti vengono discussi in modo multidisciplinare per convalidare le indicazioni chirurgiche.
Il follow-up post-operatorio della chirurgia bariatrica/per la perdita di peso è indispensabile a vita per il paziente operato, in quanto l’obesità è una malattia cronica.
Questo follow-up regolare riduce il numero di pazienti nei quali il contatto viene perso e aiuta a rilevare complicanze post-operatorie precoci o tardive, siano esse meccaniche, metaboliche o psichiatriche.
Va notato che i problemi psichiatrici/di salute mentale sono frequenti, che vanno dalla depressione al suicidio, includendo la manifestazione di dipendenze, che sono importanti da rilevare.
Infine, il follow-up post-operatorio consente di rilevare precocemente le complicanze post-chirurgiche o il fallimento effettivo della chirurgia bariatrica/per la perdita di peso, come dimostrato dalla perdita di peso insufficiente nel lungo periodo o dal guadagno di peso eventuale.
Riferimenti bibliografici
- Bariatric Surgery and Infertility: A Prospective Study.
Consalvo V, Canero A, Salsano V. Surg Technol Int. 2017 Dec 22;31:327-330.PMID: 29316601 - Depression and Suicide After Bariatric Surgery.
Müller A, Hase C, Pommnitz M, de Zwaan M.Curr Psychiatry Rep. 2019 Aug 13;21(9):84. doi: 10.1007/s11920-019-1069-1.PMID: 31410656 Review. - Bariatric surgery: to whom and when ?
Benaiges D, Goday A, Pedro-Botet J, Más A, Chillarón JJ, Flores-Le Roux JA.Minerva Endocrinol. 2015 Jun;40(2):119-28. Epub 2015 Feb 10.PMID: 25665592 - The history of metabolic and bariatric surgery: Development of standards for patient safety and efficacy.
Phillips BT, Shikora SA.Metabolism. 2018 Feb;79:97-107. doi: 10.1016/j.metabol.2017.12.010. Epub 2018 Jan 5.PMID: 29307519