Sleeve Gastrectomy (Gastrectomia Longitudinale)
Presentazione
La gastrectomia a manica (o Sleeve Gastrectomy) è una tecnica restrittiva proposta a pazienti con iperfagia (che mangiano molto durante i pasti). È una tecnica chirurgica bariatrica, il cui obiettivo principale è aiutare i pazienti obesi a perdere peso.
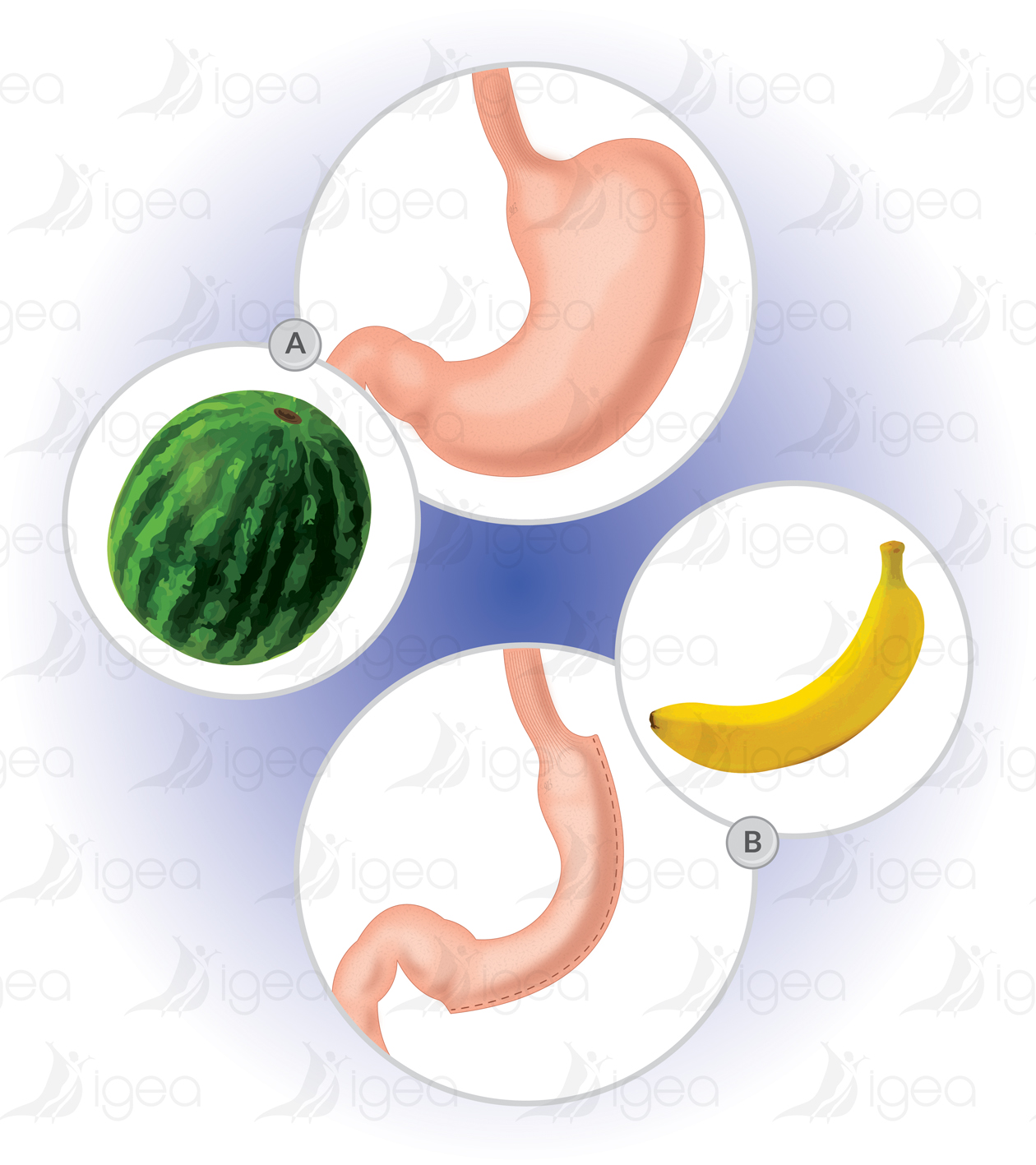
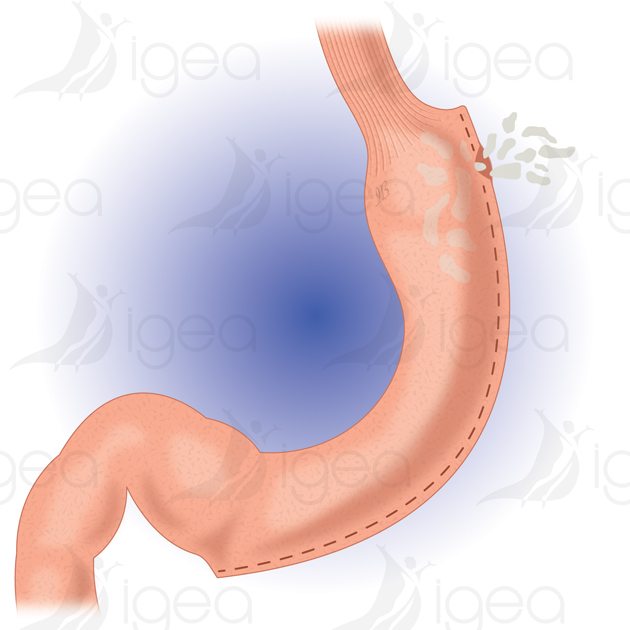
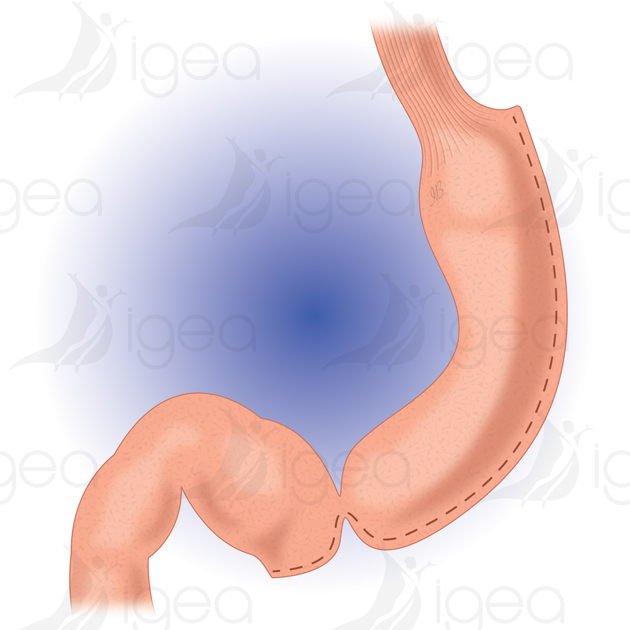
Riduzione del Volume Gastrico La procedura prevede la rimozione definitiva di 2/3 del volume gastrico, lasciando uno stomaco a forma di tubo. La resezione avviene lungo tutta la lunghezza della grande curvatura dello stomaco (circa 25-30 cm) utilizzando una sutura meccanica. Il campione gastrico rimosso viene inviato ai patologisti per l’analisi.
La grandezza dello stomaco lasciato in loco può variare a seconda del calibro del tubo gastrico utilizzato durante l’intervento (bougie). Durante l’operazione, l’anestesista inserisce un dilatatore « bougie » di 34 Fr (circa 2 cm di diametro), che garantisce uniformità nella resezione.
La tecnica è affidabile con un tasso di necessità di revisione molto basso (1-2%) nelle mani di chirurghi esperti.
Volume Gastrico Dopo Chirurgia Dopo la gastrectomia a manica, il volume residuo dello stomaco è di circa 100-150 ml (equivalente a una banana). Il follow-up post-operatorio è meno gravoso rispetto ad altre tecniche, concentrandosi sulla perdita di peso, la riduzione dell’IMC (fino a raggiungere valori normali o sovrappeso) e il miglioramento o la scomparsa di patologie legate all’obesità (diabete tipo 2, ipertensione, colesterolo/trigliceridi alti, sindrome da apnee del sonno).
Watch this surgery on Youtube
You need to be over 18 to watch this video. You must be connected to your Youtube account.
Vantaggi
- Intervento generalmente eseguito tramite laparoscopia (chirurgia a mini-invasività).
- Basso rischio di conversione in laparotomia (specialmente nei pazienti maschi super-obesi).
- Nessun corpo estraneo viene introdotto, contrariamente alla banda gastrica.
- Le graffette utilizzate sono ben integrate dopo alcuni mesi.
- Non si verificano disturbi di malassorbimento, rendendo la tecnica fisiologica.
- Nessun impatto sui farmaci, inclusi contraccettivi orali.
- Basso rischio di sindrome da dumping.
- Migliore comfort alimentare rispetto alla banda gastrica, con una dieta quasi normale possibile, sebbene in quantità ridotta.
- Non ci sono rischi di fistole o stenosi tardive come nel bypass gastrico.
- Non è necessaria una seconda chirurgia per ernie interne.
- Permette il trattamento delle comorbidità legate all’obesità con risultati simili al bypass gastrico.
Risultati
I dati pubblici riguardanti la gastrectomia a manica mostrano risultati molto interessanti a medio termine (3 anni) riguardo alla perdita di peso e alla regressione delle comorbidità.
I dati pubblici sul Sleeve Gastrectomy mostrano risultati molto positivi nel medio termine (3 anni), con una perdita di peso superiore al 60% e la regressione delle comorbidità, comparabili a quelle ottenute con il bypass gastrico. Nella nostra esperienza a Montpellier (2006-2020), la perdita di peso media è stata del 60% dopo 3-5 anni.
Esempio di paziente Una paziente obesa e diabetica sottoposta a Sleeve Gastrectomy ha perso 45 kg e ora pesa 75 kg, senza più diabete, con una qualità della vita migliorata.
Complicazioni Possibili
- Fistola: La complicazione post-operatoria più grave, con una probabilità del 3%. Si tratta di una fuoriuscita di fluido digestivo lungo la linea delle graffette.
- Emorragie Precoce: Tasso di incidenza del 2,5%, che può richiedere un intervento chirurgico nelle prime 24-48 ore.
- Stenosi: Ristrettezza anomala dello stomaco residuo, con un rischio stimato del 3%. Può causare vomito persistente.
- Reflusso Gastroesofageo (GERD): Circa il 20% dei pazienti può soffrire di GERD dopo l’intervento. Sebbene controllato con farmaci (PPI), nei casi gravi, può essere necessario un bypass gastrico.
- Dilatazione della Manica Gastrica: Più comune se il calibro della manica era troppo grande all’inizio. La dilatazione è rara se il tubo gastrico è ben calibrato e stretto.
Mortalità La mortalità di questa procedura è estremamente bassa, pari allo 0,20%, secondo uno studio che ha coinvolto 143.449 pazienti in Francia tra il 2007 e il 2012.
Conclusioni La Sleeve Gastrectomy è una tecnica chirurgica efficace per il trattamento dell’obesità, con un buon profilo di sicurezza e risultati a lungo termine. La perdita di peso media del 60-70% e la remissione di comorbidità, come il diabete e l’ipertensione, sono tra i principali benefici. Tuttavia, è necessario un attento follow-up post-operatorio per monitorare eventuali complicazioni come il reflusso gastroesofageo o la dilatazione della manica.
Una fistola è la complicanza post-operatoria peggiore della Sleeve Gastrectomy:
Comporta una perdita di liquido digestivo in un punto sulla linea di graffette (perdita di agenti di contrasto orale per opacizzazione per una scansione OGDT).
Il tasso di incidenza di questa complicanza è del 3%.
La formazione di un ascesso subfrenico sul lato sinistro dello stomaco, il quadro clinico di peritonite o emorragie precoci richiedono generalmente una nuova chirurgia entro le prime 24-48 ore.
L’apparizione di una fistola è un evento difficile da anticipare. Il quadro clinico è variabile, da una scoperta casuale a una peritonite post-operatoria.
I segni e sintomi suggestivi sono dolori addominali, dolore alla spalla sinistra (ascesso subfrenico), febbre, l’insorgenza recente di notevole difficoltà a deglutire (disfagia), vomito e, cosa più importante, un battito cardiaco anormalmente rapido, tachicardia (> 120 bpm).
La tachicardia post-operatoria semplice in una persona obesa deve essere presa sul serio: è un segno clinico di avvertimento molto specifico (Federazione di Chirurgia Viscerale e Digestiva = gestione del rischio chirurgia bariatrica).
Emorragie post-operatorie precoci
Tasso 2,5%: Sanguinamento lungo la linea delle graffette, fori dei trocar, milza e legamento gastrosplenico.
Stenosi:
Il restringimento anomalo dello stomaco residuo: si stima che questo rischio sia intorno al 3%. Nel tempo causa vomito prolungato.
Nonostante l’uso di un dilatatore di calibrazione ‘bougie’, la linea delle graffette potrebbe presentare irregolarità (un aspetto attorcigliato, spirale durante la gastroscopia). Sebbene una piccola rottura della graffetta possa non essere notata, potrebbe portare a un restringimento dello stomaco residuo. Se il problema del vomito regolare non scompare dopo una dilatazione endoscopica, è necessaria una nuova intervento chirurgico remoto. GERD (Gastroesophageal Reflux Disease): I sintomi della malattia da reflusso gastro-esofageo sono presenti in 1/3 dei pazienti, ma sono ben controllati con il trattamento medico disponibile.
Reflusso gastroesofageo:
Il 20% dei pazienti può soffrire di reflusso gastroesofageo subito dopo una Sleeve Gastrectomy.
I sintomi vengono trattati con farmaci inibitori della pompa protonica (PPI) (Omeprazolo, Pantoprazolo) con una buona risposta.
Il GERD tende a diminuire, fino a scomparire, quando il paziente perde peso in modo sufficiente.
In caso di GERD grave, può essere effettuato un bypass gastrico Roux-en-Y (RYGB).
Il tasso di mortalità di questa procedura chirurgica è praticamente zero (0,20%).
Stimiamo che attualmente la Sleeve Gastrectomy, se eseguita da un team di esperti, offra un livello di sicurezza molto alto con una bassa morbidità globale.
Complicazioni tardive della Sleeve Gastrectomy:
Dilatamento del tubo gastrico: Probabilmente legato a un difetto o a una calibrazione troppo grande all’inizio. Se tutta la grande tuberosità è stata rimossa per creare un tubo stretto, la dilatazione nel tempo è improbabile o meno probabile poiché le fibre muscolari della curvatura minore non sono molto estensibili. Tuttavia, un tubo gastrico troppo grande a livello prossimale (lasciando un aspetto diverticolare del fondo) potrebbe, teoricamente, essere predisposto a questa complicazione. Questo aspetto si riscontra talvolta in una procedura di sleeve gastrectomy dopo un band gastrico che non ha avuto successo.
Aumento di peso: È difficile attribuire l’aumento di peso a una dilatazione della gastroplastica, che rimane un evento raro. Inoltre, è stata ottenuta una notevole perdita di peso con una calibrazione relativamente grande. L’aumento di peso è più probabile se non viene seguita la dieta richiesta, con cibi ipercalorici dalla consistenza pastosa e liscia (frullati) combinati con l’assenza di attività fisica.
Riferimenti bibliografici
- Three-Trocar Sleeve Gastrectomy vs Standard Five-Trocar Technique: a Randomized Controlled Trial.
Consalvo V, Salsano V, Sarno G, Chaze I. Obes Surg. 2017 Dec;27(12):3142-3148. doi: 10.1007/s11695-017-2760-0.PMID: 28620894 Clinical Trial. - Sleeve Gastrectomy: Surgical Technique, Outcomes, and Complications.
Felsenreich DM, Bichler C, Langer FB, Gachabayov M, Prager G. Surg Technol Int. 2020 May 28;36:63-69.PMID: 32359172 - Sleeve Gastrectomy: Surgical Tips.
Chung AY, Thompson R, Overby DW, Duke MC, Farrell TM.J Laparoendosc Adv Surg Tech A. 2018 Aug;28(8):930-937. doi: 10.1089/lap.2018.0392. Epub 2018 Jul 13.PMID: 30004814 - Long term (7 or more years) outcomes of the sleeve gastrectomy: a meta-analysis
Clapp B, Wynn M, Martyn C, Foster C, O’Dell M, Tyroch A. Surg Obes Relat Dis. 2018 Jun;14(6):741-747. doi: 10.1016/j.soard.2018.02.027 - Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss in Patients With Morbid Obesity: The SM-BOSS Randomized Clinical Trial
Ralph Peterli JAMA 2018 Jan 16;319(3):255-265. doi: 10.1001/jama.2017.20897. - Laparoscopic sleeve gastrectomy and gastroesophageal reflux.
Stenard F, Iannelli A.World J Gastroenterol. 2015 Sep 28;21(36):10348-57. doi: 10.3748/wjg.v21.i36.10348.PMID: 26420961 - Laparoscopic sleeve gastrectomy: More than a restrictive bariatric surgery procedure?
Benaiges D, Más-Lorenzo A, Goday A, Ramón JM, Chillarón JJ, Pedro-Botet J, Flores-Le Roux JA.World J Gastroenterol. 2015 Nov 7;21(41):11804-14. doi: 10.3748/wjg.v21.i41.11804.PMID: 26557004 - Sleeve gastrectomy and Roux-en-Y gastric bypass are equally effective in correcting insulin resistance.
Benaiges D, Flores Le-Roux JA, Pedro-Botet J, Chillarón JJ, Renard M, Parri A, Ramón JM, Pera M, Goday A.Int J Surg. 2013;11(4):309-13. doi: 10.1016/j.ijsu.2013.02.007. Epub 2013 Feb 24.PMID: 23462580 Clinical Trial. - Challenges in the Diagnosis of Leak After Sleeve Gastrectomy: Clinical Presentation, Laboratory, and Radiological Findings.
Al Zoubi M, Khidir N, Bashah M.Obes Surg. 2020 Oct 6. doi: 10.1007/s11695-020-05008-y. Online ahead of print.PMID: 33025538 - Gastric leak after laparoscopic sleeve gastrectomy.
Márquez MF, Ayza MF, Lozano RB, Morales Mdel M, Díez JM, Poujoulet RB.Obes Surg. 2010 Sep;20(9):1306-11. doi: 10.1007/s11695-010-0219-7.PMID: 2057478 - Gastric Stenosis After Sleeve Gastrectomy: an Algorithm for Management.
Hamed H, Elghadban H, Ezzat H, Attia M, Sanad A, El Sorogy M.Obes Surg. 2020 Dec;30(12):4785-4793. doi: 10.1007/s11695-020-04858-w. Epub 2020 Jul 18.PMID: 32683638 - Portomesenteric vein thrombosis after laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass: a 36-case series.
El Lakis MA, Pozzi A, Chamieh J, Safadi B.Surg Endosc. 2017 Mar;31(3):1005-1011. doi: 10.1007/s00464-016-5078-4. Epub 2016 Jul 7.PMID: 273871 - Pancreatitis following bariatric surgery.
Baran KC, de Brauw M.BMC Surg. 2019 Jul 5;19(1):77. doi: 10.1186/s12893-019-0532-6.PMID: 31277624 - Weight Regain Following Sleeve Gastrectomy-a Systematic Review.
Lauti M, Kularatna M, Hill AG, MacCormick AD.Obes Surg. 2016 Jun;26(6):1326-34. doi: 10.1007/s11695-016-2152-x.PMID: 27048439 - Does Sleeve Gastrectomy Expose the Distal Esophagus to Severe Reflux?: A Systematic Review and Meta-analysis.
Yeung KTD, Penney N, Ashrafian L, Darzi A, Ashrafian H.Ann Surg. 2020 Feb;271(2):257-265. doi: 10.1097/SLA.0000000000003275.PMID: 30921053