Bypass gastrico Roux-en-Y (RYGB)
Bypass gastrico en Y
Presentazione
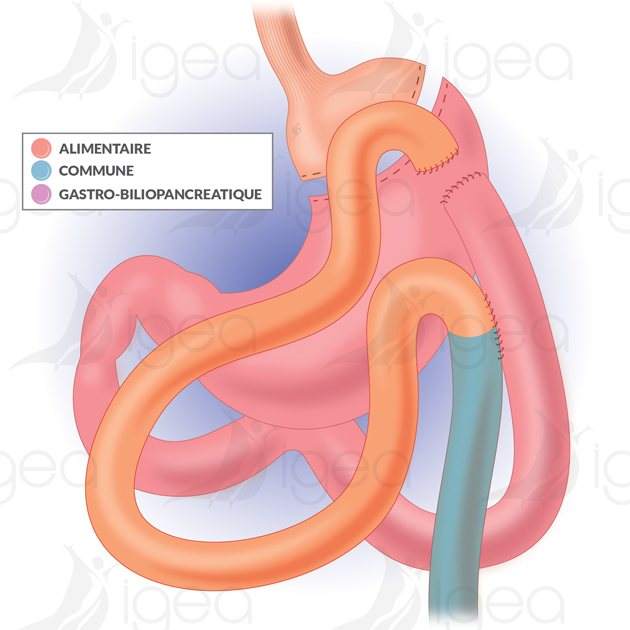
Il Gastric Bypass consiste nel creare una piccola tasca gastrica nella quale arrivano i cibi:
- Questa tasca ha una capacità ridotta di 30-50 ml, che consente solo piccoli pasti (restrittiva).
- Riduzione dell’assunzione calorica
- Meno digestione degli alimenti da parte del nuovo stomaco.
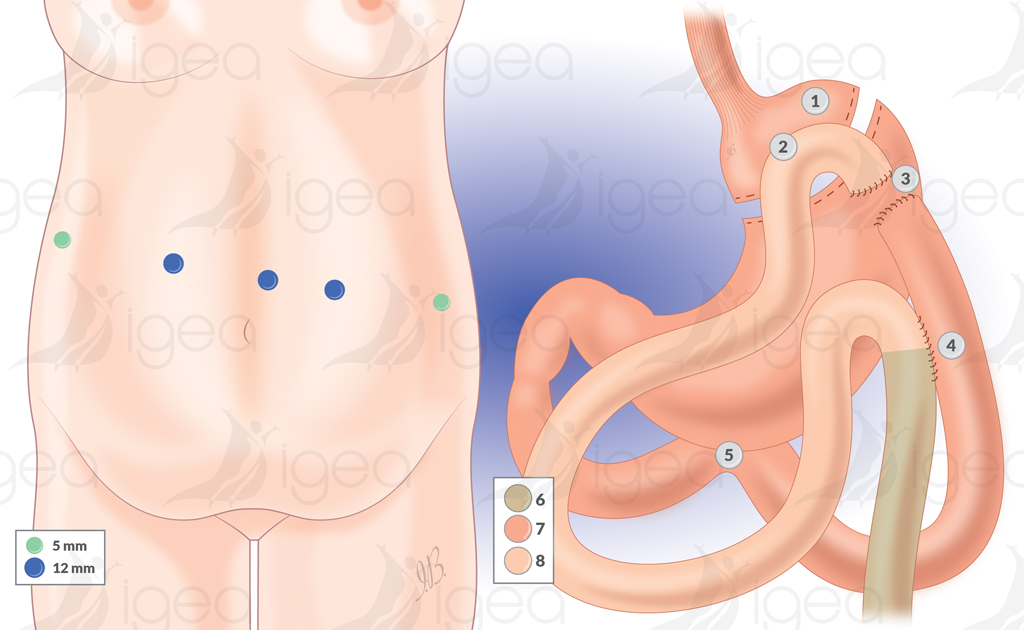
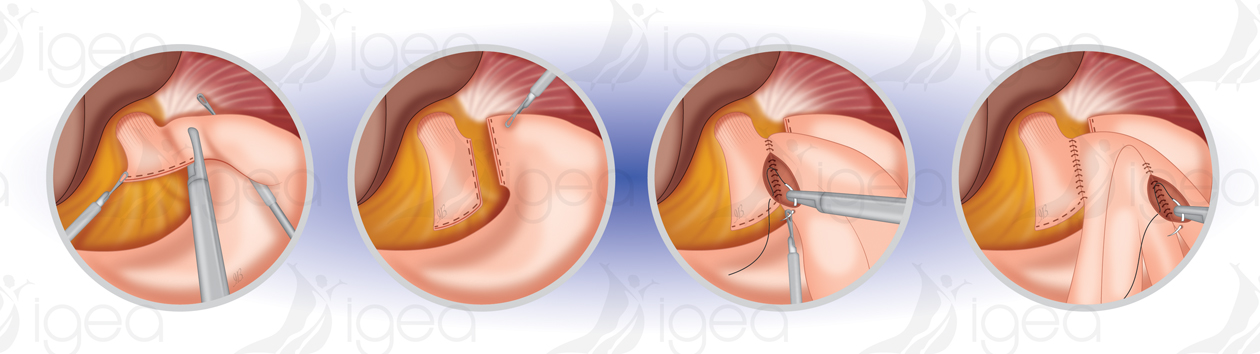
Questa tasca è collegata direttamente al digiuno (« 1 » anastomosi gastro-digiunale latero-laterale):
- Il cibo passa nell’intestino, bypassando gran parte dello stomaco, del duodeno e del digiuno:
- Segmento dell’intestino tenue escluso (malassorbimento) – ↓ calorie e nutrienti:
- Ormoni intestinali:
- Sazietà precoce
- Soppressione dell’appetito
- Inversione del meccanismo principale del diabete di tipo 2.
Viene realizzata una seconda anastomosi a 150 cm di distanza (anastomosi 2 = anastomosi latero-laterale jéjunale-jéjunale) per consentire il passaggio delle secrezioni bilio-pancreatiche:
- La sezione del tratto bilio-pancreatico a sinistra dell’anastomosi G-J consente la terminazione/conversione del Omega Loop Gastric Bypass in Roux-en-Y Gastric Bypass.
- La chiusura sistematica delle brecce mesenteriche aiuta a ridurre il rischio di ernia interna, che di solito appare nei primi 2 anni dopo un LRYGBP, dopo una perdita di peso significativa e la riduzione del mesentere.
Il Bypass aiuta a ridurre l’assunzione calorica e anche l’assorbimento delle sostanze nutritive. È una chirurgia a effetto misto: restrizione e malassorbimento
Perché scegliere il Bypass: 7 punti
Il gastric bypass come intervento chirurgico di riferimento (gold standard) in caso di obesità morbida.
- Il gastric bypass è la chirurgia bariatrica/peso-limite più efficiente in termini di risultati di perdita di peso.
- Dopo l’ablatione della banda gastrica (il tasso di fistole del bypass è inferiore a quello della sleeve gastrectomy).
- Dopo il fallimento della sleeve gastrectomy (il tasso di fistole del bypass è inferiore a quello della sleeve gastrectomy).
- Dopo sleeve gastrectomy con una persona molto obesa – BMI >50 Kg/m2 (chirurgia in due fasi).
- Con un paziente obeso che soffre di GORD (il bypass = il miglior trattamento per il reflusso) rispetto a una sleeve gastrectomy.
- Con un paziente obeso anche diabetico (un bypass è il miglior trattamento per le persone obese e diabetiche).
- Con pazienti obesi con abitudini alimentari anarchiche, tra cui snack dolci regolari e la nozione di consumare grandi quantità di bibite gassate (« dumping syndrome »).
Perdita di peso spiegata da 4 meccanismi:
- Dimensioni ridotte della tasca gastrica (30-50 cc).
- L’importanza del malassorbimento varia in relazione alla lunghezza del digiuno escluso.
- Riduzione del tasso dell’ormone ghrelin e modifiche dei tassi degli ormoni intestinali (aumento di GLP-1, PYY e oxyntomodulina, riduzione di GIP):
- Sazietà precoce
- Soppressione dell’appetito
- Inversione del meccanismo principale del diabete di tipo 2.
- Dumping syndrome associata all’ingestione di cibi dolci (malessere, diarrea, sudorazione).
Il gastric bypass è la chirurgia bariatrica più efficace per la perdita di peso in termini di risultati.
Vantaggi
- Perdita di peso sostanziale.
- Miglioramento rapido della qualità della vita.
- Il comfort alimentare è migliore con una gastroplastica (i vomiti sono rari).
Risultati valutati a lungo termine:
- Perdita di peso dopo 5-10 anni.
- 60-70% (% perdita di peso in eccesso).
- Remissione del diabete.
- Controllo di altri disturbi legati all’obesità.
Svantaggi del Bypass :
- Chirurgia tecnicamente più difficile = il tempo di chirurgia rimane breve se eseguita da un « chirurgo esperto ».
- Rischio di carenza vitaminica = la digestione delle vitamine « liposolubili » è ridotta (vitamine A, D, E, K), vitamina B12 e altri nutrienti e oligoelementi.
- I risultati in termini di perdita di peso, regressione delle comorbidità, gestione di eventuali complicazioni con interventi remoti e soddisfazione del paziente dipendono dall’impegno del paziente a seguire un protocollo di follow-up di qualità.
Risultati
La percentuale di perdita di peso in eccesso ottenuta con il Roux-en-Y gastric bypass (RYGB) – a medio termine – è significativa (%EWL = 90%) e rimane stabile dopo cinque anni con un basso tasso di effetti secondari (10-15%).
- Con la tua piccola tasca gastrica (volume di circa 50cc), mangerai quantità più piccole a ogni pasto.
- Mangiare troppo o troppo velocemente può provocare vomito o dolore intenso.
- La quantità di cibo che puoi mangiare aumenterà progressivamente, ma rimarrà sempre piccola.
- La perdita di peso a lungo termine dopo un gastric bypass dipenderà dal tuo impegno. Dovrai mantenere i cambiamenti nelle tue abitudini alimentari e fare esercizio fisico.
- I miglioramenti osservati in termini di diabete di tipo 2, pressione alta e ipercolesterolemia (colesterolo elevato) possono ridurre considerevolmente il rischio di avere un attacco cardiaco o un ictus.
Risultati a lungo termine di un LRYGB gastric bypass :
Il risultato finale a lungo termine dipende dal mantenimento di uno stile di vita sano, in termini di abitudini alimentari (raccomandiamo alimenti a basso contenuto di zucchero e alimenti vegetariani) e di esercizio fisico.
Complicazioni possibili
La difficoltà di questa procedura chirurgica (LRYGB) risiede nella creazione di una piccola tasca gastrica e nella realizzazione di due suturazioni intestinali (anastomosi) tramite laparoscopia.
Il tasso di mortalità varia dallo 0 all’1 %.
Eseguiamo sistematicamente una scintigrafia con opacificazione orale, secondo un protocollo pubblicato nel 2017.
Complicazioni post-operatorie immediate con un bypass LRYGB :
- Fistole (rottura della sutura): 1-3%
- Emorragia: 1%.
Complicazioni tardive con un bypass LRYGB :
- Ulcera anastomotica (a volte con perforazione e pneumoperitoneo): 4%.
- Stenosi dell’anastomosi gastro-digiunale: 2%.
- Ernia interna (occlusione intestinale): 2,5 %.
- Calcoli alla vescica (che richiedono una colecistectomia).
Complicazioni metaboliche con un bypass LRYGB :
- Carenze nutrizionali (evitare la carenza di vitamina B12).
- Ipossoemia dopo un pasto (sindrome da dumping).
Riferimenti bibliografici
- Metabolic effects and outcomes of sleeve gastrectomy and gastric bypass: a cohort study.
Calvo B, Gracia JA, Bielsa MA, Martínez M.Surg Endosc. 2020 Dec;34(12):5550-5557. doi: 10.1007/s00464-019-07355-z. Epub 2020 Jan 13.PMID: 31932931 - Procedure and outcomes of Roux-en-Y gastric bypass.
Carlos do Rego Furtado L.Br J Nurs. 2010 Mar 11-24;19(5):307-13. doi: 10.12968/bjon.2010.19.5.47083.PMID: 20335900 - Simulation-based training and learning curves in laparoscopic Roux-en-Y gastric bypass.
Zevin B, Aggarwal R, Grantcharov TP.Br J Surg. 2012 Jul;99(7):887-95. doi: 10.1002/bjs.8748. Epub 2012 Apr 18.PMID: 2251122 - Intraoperative iodinated contrast swallow with CT-scan delayed control for detection of early complications in laparoscopic gastric bypass: A case series of 260 cases
Vincenzo Consalvo MD , Vincenzo Salsano MD, Gerardo Sarno MD
Internation journal of surgery open , vol 7 ,pag 1-4 , 2017
https://doi.org/10.1016/j.ijso.2017.03.001 - Prevalence of Dumping Syndrome After Laparoscopic Sleeve Gastrectomy and Comparison with Laparoscopic Roux-en-Y Gastric Bypass.
Ahmad A, Kornrich DB, Krasner H, Eckardt S, Ahmad Z, Braslow A, Broggelwirth B.Obes Surg. 2019 May;29(5):1506-1513. doi: 10.1007/s11695-018-03699-y.PMID: 30635813 - The Effect of Dumping on Weight Loss in Conversion of Failed Restrictive Surgery: a Cross-Sectional Pilot Study.
Van Looveren R, Mandeville Y, Logghe P, Vandendriessche K, Verbeke X, Vuylsteke P, Pattyn P, Smet B.Obes Surg. 2018 Mar;28(3):665-670. doi: 10.1007/s11695-017-2906-0.PMID: 28933032 - Laparoscopic Roux-en-Y gastric bypass for recalcitrant gastroesophageal reflux disease in morbidly obese patients.
Perry Y, Courcoulas AP, Fernando HC, Buenaventura PO, McCaughan JS, Luketich JD.JSLS. 2004 Jan-Mar;8(1):19-23.PMID: 14974657 - Laparoscopic conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: indications and preliminary results.
Iannelli A, Debs T, Martini F, Benichou B, Ben Amor I, Gugenheim J.Surg Obes Relat Dis. 2016 Sep-Oct;12(8):1533-1538. doi: 10.1016/j.soard.2016.04.008. Epub 2016 Apr 12.PMID: 27425833 - Roux-en-Y Gastric Bypass as a Treatment for Barrett’s Esophagus after Sleeve Gastrectomy.
Felsenreich DM, Langer FB, Bichler C, Eilenberg M, Jedamzik J, Kristo I, Vock N, Gensthaler L, Rabl C, Todoroff A, Prager G.Obes Surg. 2020 Apr;30(4):1273-1279. doi: 10.1007/s11695-019-04292-7.PMID: 31808119 - Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial
Geltrude Mingrone , Francesco Rubino
Lancet 2015 Sep 5;386(9997):964-73. doi: 10.1016/S0140-6736(15)00075-6. - Is routine cholecystectomy required during laparoscopic gastric bypass?
Villegas L, Schneider B, Provost D, Chang C, Scott D, Sims T, Hill L, Hynan L, Jones D.Obes Surg. 2004 Feb;14(2):206-11. doi: 10.1381/096089204322857573.PMID: 15018749 - Pancreatitis following bariatric surgery.
Baran KC, de Brauw M.BMC Surg. 2019 Jul 5;19(1):77. doi: 10.1186/s12893-019-0532-6.PMID: 31277624 - Internal Hernia After Laparoscopic Gastric Bypass: Effect of Closure of the Petersen Defect – Single-Center Study.
Blockhuys M, Gypen B, Heyman S, Valk J, van Sprundel F, Hendrickx L.Obes Surg. 2019 Jan;29(1):70-75. doi: 10.1007/s11695-018-3472-9.PMID: 3016798 - Cross-sectional long-term micronutrient deficiencies after sleeve gastrectomy versus Roux-en-Y gastric bypass: a pilot study.
Alexandrou A, Armeni E, Kouskouni E, Tsoka E, Diamantis T, Lambrinoudaki I.Surg Obes Relat Dis. 2014 Mar-Apr;10(2):262-8. doi: 10.1016/j.soard.2013.07.014. Epub 2013 Aug 12.PMID: 24182446 - The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults.
Golzarand M, Toolabi K, Farid R.Surg Endosc. 2017 Nov;31(11):4331-4345. doi: 10.1007/s00464-017-5505-1. Epub 2017 Apr 4.PMID: 28378086