Rimozione della colecisti (Colecistectomia)
Definizione di Colecistectomia
La colecistectomia è l’intervento chirurgico durante il quale vengono rimossi la colecisti e i calcoli che contiene.
Questa operazione richiede un breve soggiorno in ospedale ed è considerata un intervento ambulatoriale, se l’infiammazione della colecisti non è troppo grave. In questo caso, il paziente subisce l’operazione al mattino e può tornare a casa la sera stessa.
Se la colecisti è molto infiammata (come nel caso di una « colecistite »), o se il paziente è fragile e ha malattie croniche multiple, le cure chirurgiche saranno convenzionali, con un soggiorno in ospedale che va da 3 a 6 giorni.
Le indicazioni per eseguire la colecistectomia tramite laparoscopia (colecistectomia laparoscopica) sono le seguenti:
- Litiasi della colecisti sintomatica (coliche biliari)
- Litiasi complicata della colecisti
- Colecistite acuta
- Colecistite cronica
- Pancreatite dovuta a migrazione litiasica
- Litiasi delle vie biliari
Indicazioni per la Colecistectomia: quando rimuovere la colecisti ?
La colecistectomia è un intervento chirurgico che prevede la rimozione della colecisti e dei calcoli in essa contenuti. Le indicazioni per eseguire una colecistectomia tramite laparoscopia (colecistectomia laparoscopica) sono le seguenti:
- Litiasi sintomatica della colecisti (coliche biliari)
- Litiasi complicata della colecisti
- Colecistite acuta
- Colecistite cronica
- Pancreatite causata dalla migrazione litiasica
- Litiasi delle vie biliari
Litiasi della Colecisti:
La litiasi della colecisti è definita dalla presenza di calcoli nella colecisti. Le donne sono più frequentemente colpite da questa patologia. L’obesità e il diabete favoriscono la formazione di questi calcoli, che spesso sono costituiti da colesterolo.
La litiasi della colecisti può essere sintomatica, e i pazienti possono soffrire di periodi di dolore intenso causati da coliche biliari, dovute alla distensione della colecisti sopra un calcolo situato nel collo della colecisti o nel dotto cistico.
Dolore tipico da colica biliare:
- Il dolore è spesso l’unico sintomo, ma può essere accompagnato da nausea e vomito.
- Il dolore si verifica talvolta durante la notte e può iniziare improvvisamente, tipicamente dopo un pasto pesante (mangiare cibi grassi e alcol).
- Il dolore è localizzato sotto le costole sul lato destro (ipocondrio destro) o al centro dell’addome superiore (epigastrio).
- Il dolore può impedire la respirazione (inibizione inspiratoria: segno di Murphy spontaneo) e irradiarsi verso il quadrante superiore destro o tra le spalle.
- Il dolore aumenta per circa un’ora, poi diminuisce.
Tutte le coliche biliari che durano più di 5 ore probabilmente indicano una complicazione: colecistite, colangite o pancreatite acuta.
Nota Importante:
- Gli attacchi di coliche biliari richiedono una visita dal medico.
- Un esame clinico, una valutazione biologica e un’ecografia permettono di fare una diagnosi precisa e di confermare l’indicazione per una colecistectomia.
- L’ecografia è affidabile per individuare i calcoli della colecisti e segni di complicazioni: colecistite, migrazione del calcolo nelle vie biliari, pancreatite biliare.
Colecistite Acuta:
La colecistite è un’infiammazione (infezione) della parete della colecisti che contiene i calcoli. Più frequentemente viene chiamata colecistite calcolosa.
Possiamo distinguere tre fasi:
- Infiammazione e edema della colecisti: idrocolecisti.
- Infezione del dotto biliare (batteri intestinali): colecistite settica o piocolecisti.
- Necrosi ischemica della parete della colecisti: colecistite gangrenosa.
Sintomatologia della colecistite:
- Febbre (> 38,5° C)
- Dolore nella parte superiore destra dell’addome che si irradia verso la schiena e la zona della spalla destra
- Nausea e vomito
Spesso è necessario il ricovero in ospedale con una dieta speciale e antibiotici.
La valutazione biologica può mostrare una sindrome infiammatoria, come un aumento dei globuli bianchi e della proteina C-reattiva (CRP).
L’esame di riferimento è l’ecografia addominale, che mostrerà una colecisti con calcoli e pareti ispessite, raddoppiate di spessore e laminate.
È frequente la presenza di un versamento di liquido peri-vesicolare.
La colecisti, nel caso di colecistite, può, eccezionalmente, perforarsi, portando a una peritonite biliare.
Tutti i casi di colecistite cronica diagnosticata devono essere operati!
Se possibile, l’intervento dovrebbe avvenire tra le 48-72 ore dall’inizio del dolore acuto.
Questa chirurgia potrebbe diventare delicata a causa del fenomeno infiammatorio del peduncolo epatico e delle aderenze con organi vicini come il duodeno o l’angolo colico destro.
Colecistite Cronica:
La colecistite cronica è secondaria a una successione di colecistiti a basso volume non trattate chirurgicamente, che si sono risolte spontaneamente o con antibiotici.
L’infiammazione cronica può evolvere in:
- Colecistite cronica scleroatrofica: la colecisti è ridotta di dimensioni, la parete è ispessita e modellata intorno al calcolo.
- Colecistite cronica con pareti molto fibrose, con depositi di calcio al centro, detta anche “colecisti porcelanosa”, con il rischio di trasformazione maligna in cancro della colecisti.
- Fistola biliodigestiva / colecistoduodenale / colecistocolica: questa comunicazione tra la colecisti (o il dotto biliare) e il tubo digerente complica circa l’1-2% dei casi di colecistite cronica. Una fistola biliodigestiva è sospettata prima di ripetuti attacchi di colecistite e della presenza di aria nel dotto biliare (pneumobilia).
- Ileus biliare: è un’ostruzione intestinale causata dal movimento di un calcolo biliare fino all’ultimo anello intestinale (valvola ileocecale bloccata).
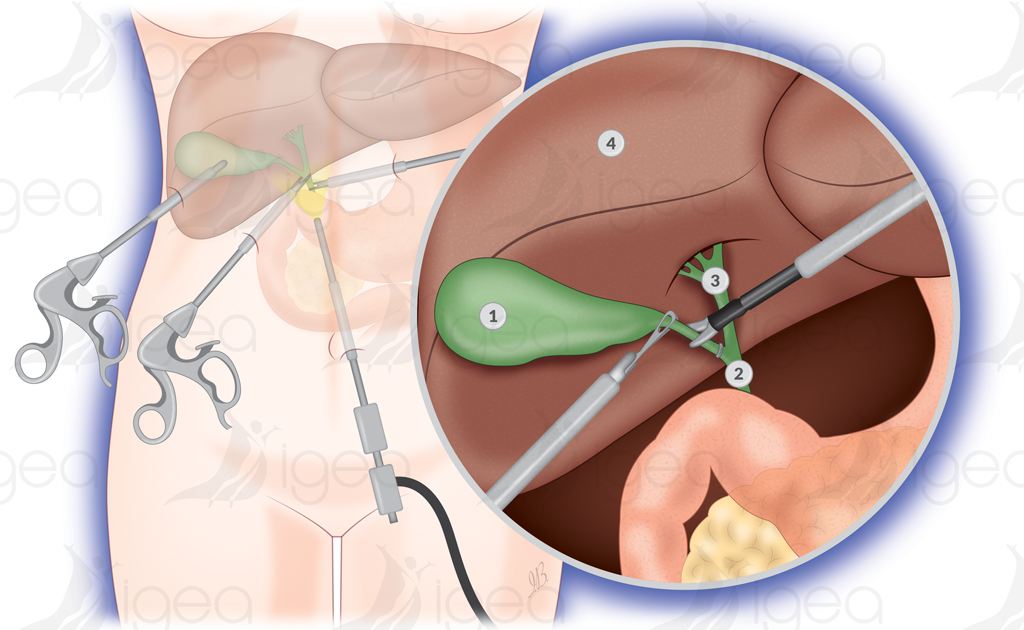
Colecistectomia Laparoscopica Ambulatoriale: la tecnica
La colecistectomia viene eseguita sotto anestesia generale, quindi il paziente non sarà cosciente durante l’intervento.
Vengono praticate 3 o 4 piccole incisioni nell’addome per la colecistectomia laparoscopica. Un tubo con una minuscola telecamera viene inserito nell’addome attraverso una delle incisioni. Questo ci permette di vedere le immagini su uno schermo nella sala operatoria e di controllare ogni nostro movimento.
Gli strumenti chirurgici vengono introdotti attraverso le altre incisioni nell’addome e la colecisti viene rimossa.
La colecistectomia laparoscopica dura da 30 minuti a due ore.
Nel caso di una colecistectomia laparoscopica, il paziente è generalmente autorizzato a tornare a casa lo stesso giorno dell’intervento, tuttavia, in alcuni casi potrebbe essere necessario rimanere in clinica per una o due notti.
In generale, verrà permesso di tornare a casa quando si sarà in grado di mangiare e bere senza dolore e camminare senza assistenza.
Di solito ci vogliono circa una settimana per recuperare completamente.
Colangiografia Peri-operatoria
Una colecistectomia sicura prevede la dissezione degli elementi del Triangolo di Calot (o Triangolo Cistoepatico) con estrema prudenza.
Il dotto cistico e l’arteria cistica vengono identificati.
Nessun elemento viene sezionato prima di eseguire una colangiografia, che è una radiografia (raggi X) dell’albero biliare (colangiogramma).
Questo aiuta a rilevare la litiasi del dotto biliare, a verificare l’assenza di lesioni al dotto biliare e a intervenire tempestivamente nel caso si presentino lesioni iatrogene.
L’importanza dell’esplorazione radiologica per scoprire lesioni iatrogene nel dotto biliare principale durante una colecistectomia, e per prevenire effetti indesiderati gravi, è confermata dalla letteratura medica.
La colangiografia può essere eseguita su base elettiva (anatomia difficile; potenziale litiasi) o in modo sistematico.
Rischio di Conversione
La colecistectomia laparoscopica non è adatta per tutti.
In alcuni casi, il chirurgo potrebbe iniziare con un approccio laparoscopico e poi decidere di convertire l’intervento in laparotomia.
La decisione di convertire in laparotomia (praticando un’incisione più grande) viene presa in presenza di cicatrici da operazioni precedenti o a causa di complicazioni.
Colecistectomia Chirurgica Tradizionale (Apertura)
Durante una colecistectomia tradizionale (aperta), il chirurgo eseguirà un’incisione di circa 10 cm nell’addome, sotto le costole, sul lato destro.
I muscoli e i tessuti vengono spostati verso la parte posteriore per esporre il fegato e la colecisti. Successivamente, il chirurgo procederà con l’operazione. L’incisione verrà chiusa con dei punti di sutura alla fine.
Questo intervento dura tra 1 e 2 ore.
Dopo la colecistectomia, il paziente verrà portato in una sala di recupero o in un’unità di cura post-anestesia (PACU) per riprendersi in modo sicuro dall’anestesia e ricevere la cura post-operatoria adeguata. Successivamente, il paziente verrà trasferito nella sua stanza. Il tempo di recupero può variare, a seconda della tecnica chirurgica utilizzata e delle condizioni di salute del paziente.
Nel caso di una colecistectomia tradizionale, potrebbe essere necessario rimanere in ospedale per due o tre giorni per il convalescenza. Una volta a casa, potrebbero volerci dalle quattro alle sei settimane per un completo recupero.
Complicazioni potenziali con una Colecistectomia
Una colecistectomia presenta pochi rischi di complicazioni, ma queste possono includere:
Complicazioni potenziali durante il periodo peri-operatorio:
- Emorragia: un sanguinamento può verificarsi durante l’intervento, richiedendo un controllo chirurgico immediato.
- Pancreatite: l’infiammazione del pancreas può essere causata da una lesione dei dotti biliari o da un blocco del flusso biliare.
- Lesioni iatrogene degli organi adiacenti: durante l’intervento, possono verificarsi danni ai dotti biliari, al fegato o all’intestino tenue.
- Perdite di bile: sebbene le lesioni iatrogene dei dotti biliari siano meno frequenti con la chirurgia aperta, il rischio di perdite di bile rimane maggiore con la laparoscopia, anche se negli ultimi anni i tassi sono diminuiti. Nel 2020, la percentuale di lesioni iatrogene dei dotti biliari era ancora due volte più alta con la colecistectomia laparoscopica rispetto a quella aperta.
Complicazioni a medio/lungo termine:
- Colangite con calcoli residui: se alcuni calcoli biliari non vengono rimossi durante l’intervento, possono provocare un’infezione del sistema biliare.
- Stenosi del dotto biliare principale: una cicatrizzazione o un restringimento dei dotti biliari che può causare problemi al flusso della bile.
Rischio di complicazioni Il rischio di complicazioni dipende dalle condizioni generali di salute del paziente e dalle ragioni per cui viene eseguita la colecistectomia. Ad esempio, pazienti con comorbidità o patologie croniche potrebbero essere a rischio maggiore di complicazioni.
Convalescenza dopo una Colecistectomia
La colecistectomia viene eseguita per alleviare il dolore e il disagio causati dai calcoli biliari.
Alcune persone possono soffrire di leggera diarrea dopo l’intervento, ma questo sintomo generalmente scompare rapidamente.
La maggior parte dei pazienti non sviluppa problemi digestivi dopo questo tipo di chirurgia.
La colecistectomia non influisce significativamente sulla digestione, poiché la colecisti non è essenziale per questo processo. Tuttavia, è consigliabile limitare il consumo di cibi grassi nelle due settimane successive all’intervento per favorire una migliore guarigione e ridurre eventuali fastidi.
Recupero dopo la Colecistectomia laparoscopica:
Dopo una colecistectomia laparoscopica (chirurgia a cielo chiuso), i pazienti di solito possono tornare al lavoro dopo pochi giorni, se la convalescenza procede senza complicazioni.
Recupero dopo Colecistectomia aperta:
Nel caso di una colecistectomia aperta, il periodo di convalescenza è più lungo, e potrebbero essere necessarie due o tre settimane prima che il paziente possa tornare a lavorare. Il tempo di recupero completo può richiedere più tempo, fino a quattro o sei settimane.
Informazioni utili
Informazioni utili per prepararsi a una Colecistectomia::
-
-
Consulta il medico riguardo ai farmaci e integratori:
- Parla con il medico di tutti i farmaci e integratori che stai assumendo.
- Continua a prendere la maggior parte dei farmaci come prescritto.
- Interrompi l’assunzione di alcuni farmaci che potrebbero aumentare il rischio di sanguinamento.
-
Dieta prima dell’intervento:
- Non mangiare né bere nulla la notte prima dell’intervento. Puoi bere un sorso d’acqua con i farmaci, ma evita di mangiare e bere almeno 6 ore prima dell’intervento.
-
Preparazione pre-operatoria:
- Fai una doccia e usa sapone antibatterico prima dell’intervento.
-
Pianifica il ritorno a casa e la convalescenza:
- Trova qualcuno che ti accompagni a casa e resti con te per un po’.
- Chiedi a un amico o a un familiare di accompagnarti a casa e rimanere con te la prima notte dopo l’intervento.
- La maggior parte delle persone può tornare a casa lo stesso giorno dell’intervento, ma a volte possono verificarsi complicazioni che richiedono una permanenza in clinica per una o più notti.
- Se il chirurgo deve fare un’incisione lunga nell’addome per rimuovere la colecisti, potrebbe essere necessario un soggiorno più lungo in clinica.
- Non sempre è possibile sapere in anticipo quale procedura sarà utilizzata.
- Considera la possibilità di dover rimanere in clinica durante il periodo di recupero.
-
Cosa portare in ospedale:
- Non dimenticare di portare gli effetti personali necessari, come ad esempio un spazzolino da denti, abiti comodi e libri o riviste per il tempo libero.
Colecistectomia laparoscopica (chirurgia a cielo chiuso) – Trattamento come paziente ambulatoriale alla Clinica Clementville, Montpellier:
Dopo l’intervento:
-
Risveglio e recupero immediato:
- Una volta che ti sveglierai, sarai portato al reparto di chirurgia ambulatoriale. Un’infermiera ti offrirà un bicchiere d’acqua o una tisana. A pranzo dovrai mangiare un pasto leggero.
- Verranno somministrati tranquillanti/antidolorifici tramite una flebo, che rimarranno in posizione per 2-3 ore.
- L’infermiera controllerà l’intensità del dolore, la tua capacità di muoverti autonomamente, la ripresa della minzione e della funzione intestinale, e l’aspetto delle ferite.
-
Controllo del dolore e dimissione:
- Dopo alcune ore di recupero, la flebo verrà rimossa e gli antidolorifici saranno presi per via orale.
- Il personale infermieristico e l’anestesista assicureranno che il dolore non ritorni e che il tuo comfort addominale rimanga stabile.
- Dopo di che, potrai essere dimesso.
-
Documenti di dimissione:
- L’infermiera ti fornirà tutti i documenti necessari, inclusi:
- Il referto operatorio,
- La tua cartella clinica,
- La lettera di dimissione per il medico di base con il certificato di malattia,
- La prescrizione di farmaci da prendere a casa,
- L’appuntamento con il medico di base per una visita di controllo dopo 1 settimana,
- L’appuntamento con il chirurgo per una visita di controllo dopo 5 settimane.
- L’infermiera ti fornirà tutti i documenti necessari, inclusi:
Dimissioni dalla clinica:
- Visita di dimissione: La dimissione verrà autorizzata dopo una visita con l’anestesista (insieme al chirurgo).
- Orario di dimissione: In pratica, lascerai il reparto tra le 15:00 e le 19:00, accompagnato da un familiare.
- Prima cena a casa: Deve essere leggera, si consiglia una zuppa e uno yogurt.
Durante i giorni successivi:
-
Cura delle ferite:
- Le ferite non necessitano di particolari cure grazie alla tecnica di chiusura: sutura intradermica (sutura interna) e adesivo biologico.
-
Doccia:
- Puoi fare una doccia il giorno dopo l’intervento.
-
Certificato medico di malattia:
- Il certificato di malattia è valido per 15 giorni, ad eccezione dei lavoratori che svolgono lavori fisici attivi, per i quali è valido per 4 settimane.
-
Riferimenti bibliografici
- Reference 1 : Test1
- Reference 2 : Test
- Reference 3 : Test
- Reference 4 : Test
- Reference 5 : Test
- Reference 6 : Test
- Reference 7 : Test
- Reference 8 : Test
- Reference 9 : Test