Left colon
Definition
A cancer of the left colon is located on the left-hand part of the colon which goes from the left colic angle or sigmoid.
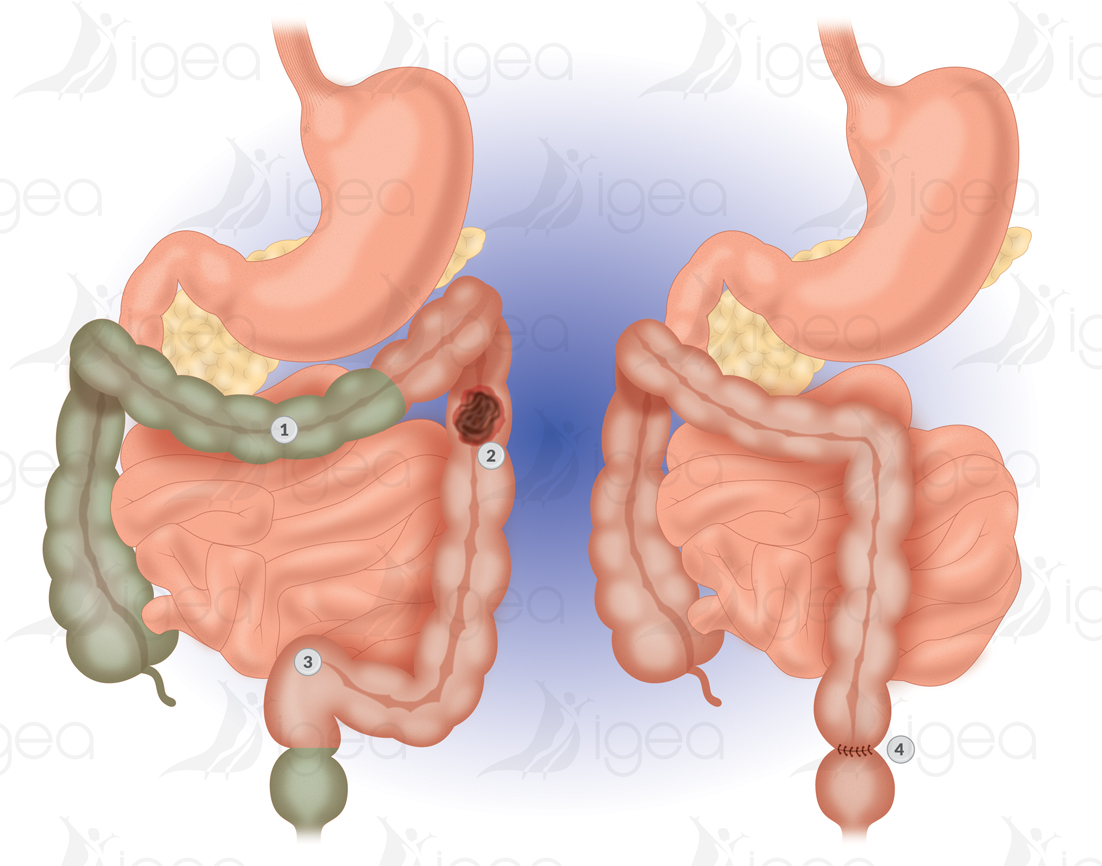
This surgical condition is treated by carrying out a left hemicolectomy.
This is a resection of the left colon, with re-establishment of digestive continuity.
This is carried out with a suture (colo-colonic anastomosis) between the left proximal colon (or the transverse colon) and the sigmoid colon (or rectum).
Risk factors
Polyps :
Between 60 and 80 % of cancers of the colon develop on precancerous benign tumours polyps or adenomas. The frequency of such lesions regularly increases with age. As shown by observations at autopsies, 12% of people under 55 have such a condition.
Age :
Colon cancers are rare before 40 years of age.
Heredity :
Globally, if a first-degree parent has a cancer, it multiplies by two the risk of contracting a cancer.
Family Syndromes :
Certain family illnesses carry a major risk of colon cancer. In particular cases of adenomatous polyposis in the family, which is characterised by the early appearance of multiple polyps all over the colon, and the Lynch syndrome (also known as hereditary non-polyposis colorectal cancer – HNPCC).
The early development of a cancer is inevitable with familial polyposis.
With the Lynch syndrome the risk is extremely high, but comes a little later. It is associated with an increase in the frequency of endometrial cancers as well as, less frequently, other cancers (stomach, ovaries, urinary tract… )
MICI (chronic inflammatory bowel disease) :
The influence of Crohn’s disease on cancer of the colon has remained controversial for a long time.
Ulcerative colitis is a classic risk factor for colorectal cancer. However, the risk is a function of the extent to which the colon was affected over time.
Today, it is clear that this disease is also an important risk factor when it affects the whole colon, and if it started at a young age.
Food :
Other risk factors for colon cancer have been raised, such as a diet low in fibre and high in fats.
However, certain data suggests that the chronic use of nonsteroidal anti-inflammatory drugs may have a protective effect. But these factors remain very controversial.
Signs and Symptoms
Signs and symptoms of colorectal cancer can also be caused by other medical conditions.
It is important to consult a doctor if you have unusual symptoms.
- Weight loss.
- Anaemia.
- Unusual bowel movements.
- Persistent diarrhoea.
- Persistent constipation.
- Reduction in bowel movement size (caused by a partial blockage of the large intestine).
- Presence of blood on or in bowel movements, bright red, rectal bleeding between bowel movements.
- Mucus in bowel movements.
- Sense of incomplete evacuation of the intestine.
- Urgent need to go to the toilet for bowel movement.
- Abdominal discomfort or painful stomach cramps.
- Sometimes a large mass felt in the abdomen.
- Bloating, gas.
- Sensation of being full.
- Tiredness.
Surgical treatment
OPERATIVE INDICATIONS LEFT HEMICOLECTOMY OR SEGMENT RESECTION
Cancer of the left colon: left colic angle, the descending colon, sigmoid.
Colic polyp unresectable by endoscopy.
TECHNIQUE LEFT HEMICOLECTOMY OR SEGMENT RESECTION
Cancer surgery involves the exeresis of the tumour with margins of security, and the ganglions, which will be analysed to know the stage of the tumour, and propose complementary treatment (chemotherapy) if metastatic ganglions are already invasive.
An initial ligature must be made of the inferior mesenteric vein and then the inferior artery at 2cm from its origin.
Restoring continuity is made at the same time with mechanical anastomosis (manual) termino-lateral or termino-terminal.
The right colic resection is made, either by using a traditional technique, or by laparoscopy (coelioscopy, no open surgery).
The surgical act takes longer with a laparoscopy than with traditional open surgery.
The renewal of bowel movements and food intake are probably more rapid after a left colectomy using laparoscopy (coelioscopy).
The time spent in hospital is probably little different depending on the technique used.
There is no difference in the carcinological quality of the resection, or the quality of post-operative life, between a laparoscopy or traditional open surgery.
PREOPERATIVE DIET
A diet without fibre is recommended during the 8 days preceding the surgery. This is to prepare the intestine.
BOWEL PREPARATION
Prescribed to be taken at home (CitraFleet 2 sachets ) to be completed the day before surgery at the clinic with a bowel cleansing.
Complications
Complications are rare as it is surgery which is carried out regularly.
The technique, either by laparoscopyor by open surgery, is standardised, safe and reliable.
An anastomotic fistula is a major complication after a colon resection.
The risk of contracting a symptomatic anastomotic fistula is comparable whether after a right hemicolectomy or after a left hemicolectomy. The risk of contracting a fistula is estimated at between 1% and 3%.
It is a leakage of matter via the colon stitching, as the stitches are not hermetic.
This fistula may cause post-operative peritonitis, which requires urgent surgery and sometimes the creation of a double barrel stoma (temporary artificial anus 3-6 months) with disassembly of the anastomosis (Hartmann’s procedure).
Intestinal occlusion
Blocking of the small intestine.
Difficulty restarting bowel movement may make it necessary to undergo a scan to eliminate the diagnosis of a post-operative bowel obstruction with fibrous adhesions or an internal hernia (blocking of a loop of the small intestine in a gap created by the surgery)
Abscess of the abdominal wall
Rare after laparoscopic surgery.
Other risks are inherent to all types of abdominal surgery.
Haemorrhage.
Damage to another abdominal organ.
Lesion or section of the left ureter is rare. In the case of a major inflammation of the tumour adhering to the ureter.
Lesion of the spleen is rare. Such a lesion can happen when it is difficult to mobilise the left angle. The problem manifests itself through post-operative bleeding (a fall in the rate of haemoglobin). If the lesion is important and it creates substantial post-operative bleeding (a fall in the rate of haemoglobin) further surgery may be necessary (splenectomy = removal of the spleen).
A lesion of the small intestine or another abdominal organ is damaged is rare.
Such a lesion can happen when it is difficult to mobilise the left angle. The problem manifests itself through post-operative bleeding (a fall in the rate of haemoglobin). If the lesion is important and it creates substantial post-operative bleeding (a fall in the rate of haemoglobin) further surgery may be necessary (splenectomy = removal of the spleen).
Infections
Urinary infections, secondary chest infection, thrombosis of the peripheral catheter, require daily post-operative surveillance, and application of preventive measures (rapid removal of urinary catheter early reaction/mobilisation, respiratory physiotherapy, removal of perfusions, early re-alimentation).
Riferimenti bibliografici
- Reference 1 : Test1
- Reference 2 : Test
- Reference 3 : Test
- Reference 4 : Test
- Reference 5 : Test
- Reference 6 : Test
- Reference 7 : Test
- Reference 8 : Test
- Reference 9 : Test