Pancreas

Definition
Pancreatic cancer starts in the tissue of your pancreas.
The pancreas is an organ located behind the stomach, in the top and back of the abdomen in the retroperitoneal space.
The pancreas is part of the digestive system and endocrine system.
It secretes enzymes which facilitate digestion, and hormones which help regulate blood sugar levels.
The liquid secreted by the pancreas contains bicarbonate and digestive enzymes: amylase, lipase, protease. They flow from the pancreas into the major central duct of Wirsung
which joins the common bile duct coming from the liver and transporting bile.
Once the food products have left the stomach, the pancreatic juices and bile help their digestion in the duodenum.
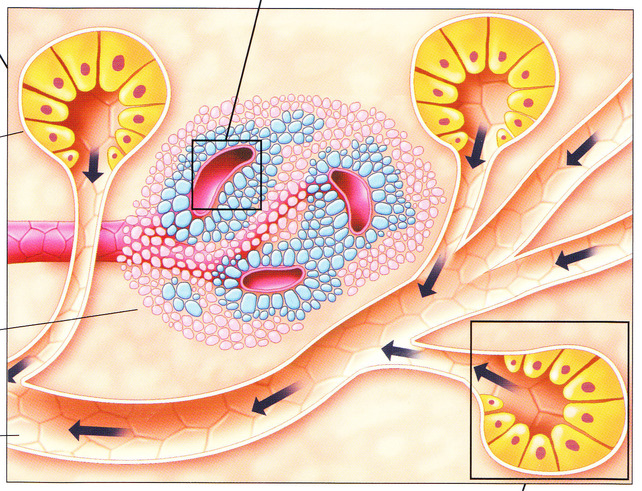
The pancreas also secretes insulin as well as glucagon and other hormones which enter the bloodstream to help the organism use and store the energy provided by food.
- Pancreatic cancer is a disease which tends to be found more often in people over 65 years old.
- Pancreatic cancer propagates generally quite rapidly.
- It is rarely detected when it starts, which is the main reason why surgical ablation is often not possible.
- Pancreatic cancer is often a bad, unwelcome diagnosis, even when diagnosed early.
Pancreatic cancer occurs when a pancreatic cell develops a genetic mutation.
These mutations provoke the uncontrolled cell growth and proliferation which makes a tumour.
The type of cells involved in a Pancreatic cancer can help determine the best treatment to give.
Types of Pancreatic cancer
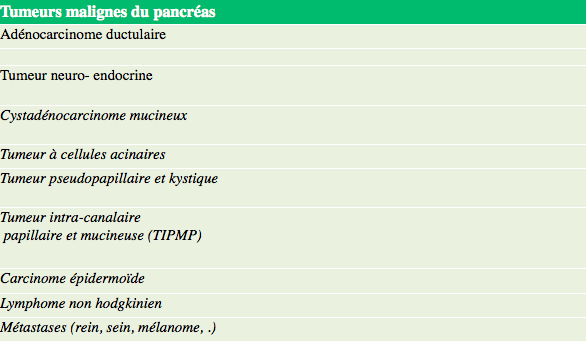
Pancreatic cancer occurs in the ducts transporting the pancreatic digestive juices.
The majority of Pancreatic cancers are Adenocarcinomas (Adenocarcinomas excreted in the pancreatic canals).
It is rare that a Pancreatic cancer starts in the endocrine cells which produce hormones.
The most frequent neuro endocrine cancers of the pancreas are the insolinomas, gastrinomas and non-functional tumours.
Risk factors
The factors which can increase the risk of developing Pancreatic cancer are as follows:
- Age > 60 ans.
- Smoking.
- Obesity
- Diet rich in fats and animal proteins (nitrates used for preserving meat).
- Chronic Pancreatitis.
- Personal or family medical history of Pancreatic cancer.
- Hereditary genetic problems such as: Lynch syndrome or hereditary non-polyposis colorectal cancer (HNPCC).
- Peutz Jeghers Syndrome mutation of the BRCA2 gene (hereditary breast and ovarian cancer).
Cancer of the pancreas may sometimes develop in the absence of all these risk factors.
Symptoms
Pancreatic cancer is often asymptomatic.
A Pancreatic cancer can grow until it is relatively large, without causing any symptoms, because the pancreas lacks nerve endings capable of sending a pain signal to the brain.
When the tumour reaches a certain dimension and starts to spread outside of the pancreas, then it can cause symptoms:
- Pain, frequency: 60-80 %. Localised pain in the region of the stomach, which may spread to the back.
- Jaundice (icterus) frequency 40-80%. The skin and the whites of the eyes take on a yellow colour, urine becomes darker as the tumour blocks the common bile duct (choledochus), and the passage of bile.
- Pruritus, frequency 25%. Severe itching and associated with icterus (jaundice).
- Weight loss, frequency 50-80 %. Weight loss is often substantial, rapid and unexplained.
- Nausea, frequency 50%.
See your GP/Family Doctor if you have unexplained weight loss, abdominal pains, a jaundice.
Health problems other than cancer can be the cause of similar signs and symptoms.
After having checked your medical history, and given you an examination, your doctor can arrange for a surgical consultation if it is considered that there is the possibility of a Pancreatic cancer.
Diagnosis
If your doctor considers there is the possibility of a Pancreatic cancer you will have several complementary examinations. The initial objective is to make a diagnosis of the tumour, and then to see if the cancer has spread (Stage analysis).
Stage analysis helps understand if the cancer can be removed surgically.
Biological Analyses
Using your blood sample, we can control in what measure your organs are functioning normally.
We check the signs and biological importance of an eventual jaundice (an increase in bilirubin, alkaline phosphatase, etc.)
A programme of certain substances (markers)are injected into your blood. They are able to be detected in the blood of people with a cancer.
The two doses of tumoural markers to detect Pancreatic cancer are the proteins CA19-9 and ACE.
The control of the marker CA19-9 is the most reliable: it is principally used to check the individual reaction to the treatment chosen for Pancreatic cancer.
Imaging techniques
These techniques provide an in-depth examination of tissue, organs and bones.
An echography uses high-frequency ultrasound to create moving images of internal organs, including the gall bladder, bile ducts and the pancreas.
The (Computerized Tomography) CT scanner and the (Magnetic Resonance Imagery) MRI scan are different techniques used with the aim to obtain an image of the tumour and check to see if it has spread.
The MRI uses a powerful magnetic field and radio waves whereas the CT scanner uses X-rays to visualise internal organs.
These tests are generally painless and require no anaesthesia.
In certain cases, you may receive an injection of a colourant (iodinated contrast, gadolinium) in a vein in your arm to help highlight the zones your radiologist wants to see.
Endoscopy
An Endoscopy allows the doctor to examine the interior of certain parts of the body by using an endoscope, which is a straight but flexible tube, which has a light and a very small camera at the end.
The diagnosis of Pancreatic cancer may require one of the following endoscopic interventions:
ERCP – Endoscopic retrograde cholangiopancreatography
A thin but flexible tube, an endoscope, is introduced into the throat to descend to the stomach, the duodenum and finally arrive at the opening of the pancreatic canal (papilla).
The gastroenterologist can then use the endoscope to inject a contrast product and take radiographic images. They show any anomaly or blockage of the bile ducts and the pancreatic canals.
If the tumour obstructs the bile ducts or the duodenum, the gastroenterologist can, with the help of the endoscope, install a small metal tube (called an endoprosthesis or stent) in order to clear the opening.
This procedure requires a general anaesthetic.
ENDOSCOPIC ULTRASOUND
The echographic sensor (and ultrasound device) is passed along an endoscope in the stomach to obtain images.
This examination can also take samples of tumoural cells (biopsy by endoscopy echo) to obtain the histological proof that the tumour exists.
Pancreatic biopsy
A biopsy is normally required to establish with certitude the diagnosis of cancer.
This procedure consists of taking a small sample of tissue of the pancreas to be examined under a microscope.
There are a number of ways to take a biopsy of the pancreas:
- A Biopsy can be taken by using a fine needle using the echography or scanner to direct the needle to the suspicious pancreatic lesion.
- The sample can be taken during an ERCP (Endoscopic retrograde cholangiopancreatography) or during an endoscopy.
Cancer staging and grading
Once the diagnosis of a Pancreatic cancer is confirmed, the Stage of the cancer must be determined.
This process of deciding the Stage of the Pancreatic cancer consists of defining the size of the tumour, and checking if it has spread from the pancreas, the organ where it started.
Four Stages have been defined for Pancreatic cancer.
Stage I : The cancer is localised exclusively in the pancreas. The tumour can be of variable size, but has not affected the lymphatic ganglions (lymph nodes) nor any other part of the body.
T1 = size <2cm
T2= size > 2cm
N0
Stage II : The cancer has propagated outside of the pancreas (T3) to adjacent tissue and organs, but remains surgically removable.
Lymphatic ganglions can be affected Stage II.
A = T3 , N0, M0
B= T1-3, N1, M0
Stage III : The cancer is not removable locally.
The cancer has affected the main blood vessels (mesenteric artery or coeliac trunk), and sometimes to the lymphatic ganglions in the proximity.
T4, all N, M0
Stage IV : The cancer has affected other parts of the body, such as the liver, the lungs and the abdominal cavity.
Stage IV M+
Presence of metastases
It is important to know the Stage of your cancer, we will help you to choose the treatment which suits you the best.
Surgical Treatment
Surgery
- The decision to have surgery depends on the size of the tumour and its location.
- Patients must not be operated if the tumour cannot be removed, or they would not benefit from its removal (Stage III and IV).
- During the surgery, we will proceed with a total ablation (removal) of the tumour and some of the healthy tissue around it.
- The surgery will take place with you under a general anaesthetic, and you will have to stay in hospital for several days afterwards.
- The surgical treatment of a Pancreatic cancer is a major operation, which develops major side effects and requires several weeks of convalescence.
- It is very important to consider the possible advantages and risks of this type of surgery with your surgeon and also discuss it with your GP/Family Doctor.
Surgery may allow the total removal of the pancreatic tumour (complete resection RO – absence of spreading).
Three types of surgical intervention are envisaged for a Pancreatic cancer at an early stage.
A pancreaticoduodenectomy, also known as a Whipple procedure:
This type of surgery is a major operation performed to remove cancerous tumours off the head of the pancreas (the largest part)
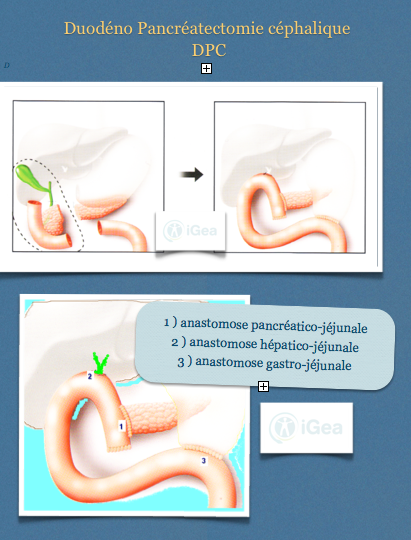
The surgeon removes:
- The head of the pancreas.
- Part of the stomach and the duodenum.
- The common bile duct and the gallbladder.
- Lymphatic ganglions (lymph nodes).
Digestive, biliary and pancreatic continuity are re-established with 3 sutures (anastomosis).
A pancreaticoduodenectomy can cause other medical conditions linked to the risk of
- Fistulas or infection (if the pancreatic–digestive suture fails).
- Post-operative haemorrhaging.
- Furthermore, a post-operative risk of death exists relative to complications.
A jejunostomy with the installation of a feeding tube direct to your intestine can be considered on a case by case basis to improve food intake. Several days can pass by before you are capable of drinking and eating correctly.
Nausea and vomiting can come back if the stomach has problems emptying (delayed gastric emptying)
After the surgery, convalescence can take a long time.
You will stay in hospital for 10-15 days, then you will stay at home for several weeks to recuperate.
After a partial or total ablation of your pancreas, you will have to take medicines to replace the enzymes which were previously made by your pancreas.
It is also possible that after a duodeno-pancreatectomy (DPC) you might become diabetic.
The diabetes will be controlled with medicines and insulin injections.
You will need to follow this treatment of substitution for the rest of your life.
Total removal of the pancreas
This type of surgery is chosen if the cancer is present in the whole of the pancreas.
The surgeon will, therefore, remove all the pancreas, part of the stomach, the duodenum, the common bile duct, the gall bladder, the spleen. and the adjacent lymphatic ganglions.
You will become diabetic after a total removal of the pancreas.
This type of surgery is not frequent.
Palliative surgery: biliary bypass and gastric bypass
In this case surgery helps to alleviate the symptoms provoked by the cancer diagnosed as being in an advanced Stage (III-IV) when it cannot be totally removed.
Biliary bypass linking the common bile duct to the small intestine in order to allow the passage of bile and alleviate the symptoms of jaundice.
Digestive bypass linking the stomach and the small intestine, to get around the blockage of the duodenum and permit normal eating and drinking.
Chemotherapy
Chemotherapy may be part if the treatment for Pancreatic cancer after surgery has taken place.
It can also be used to relieve pain or ease the symptoms if the tumour cannot be removed.
Chemotherapy can be administered in tablet form or by injection.
Chemotherapeutic medicines inhibit the development and propagation of cancer cells, but they also damage cells which are healthy.
Healthy cells can recover with time, but in the meantime, for you, the treatment will perhaps provoke certain side effects, such as: nausea, vomiting, loss of appetite, tiredness, hair loss and a higher risk of infection.
Radiotherapy (X-rays)
Radiotherapy can be used on its own or in association with chemotherapy, to continue the treatment of Pancreatic cancer instead of surgery, or after surgery (in an adjuvant situation).
It can also be used to relieve pain or ease the symptoms if the tumour cannot be removed.
Radiotherapy uses a large radiotherapy machine to aim the radiation beam precisely at the tumour. The radiation beam damages all cells in its trajectory, both cancerous and healthy.
Prognosis
Only less than 5% of all patients are alive 5 years after the diagnosis of adenocarcinoma of the head of the pancreas.
Among those patients operated to relieve pain and ease symptoms (complete resection RO), the rate of survival after 5 years is between 10 and 30 %.
The results are better if the tumour is smaller and if the cancer has not spread to ganglions (Stage I or II A).
Among the patients where the tumour is not removable, 50% are still alive 6 months after the diagnosis.
Riferimenti bibliografici
- Reference 1 : Test1
- Reference 2 : Test
- Reference 3 : Test
- Reference 4 : Test
- Reference 5 : Test
- Reference 6 : Test
- Reference 7 : Test
- Reference 8 : Test
- Reference 9 : Test