Anal abscess
Definition
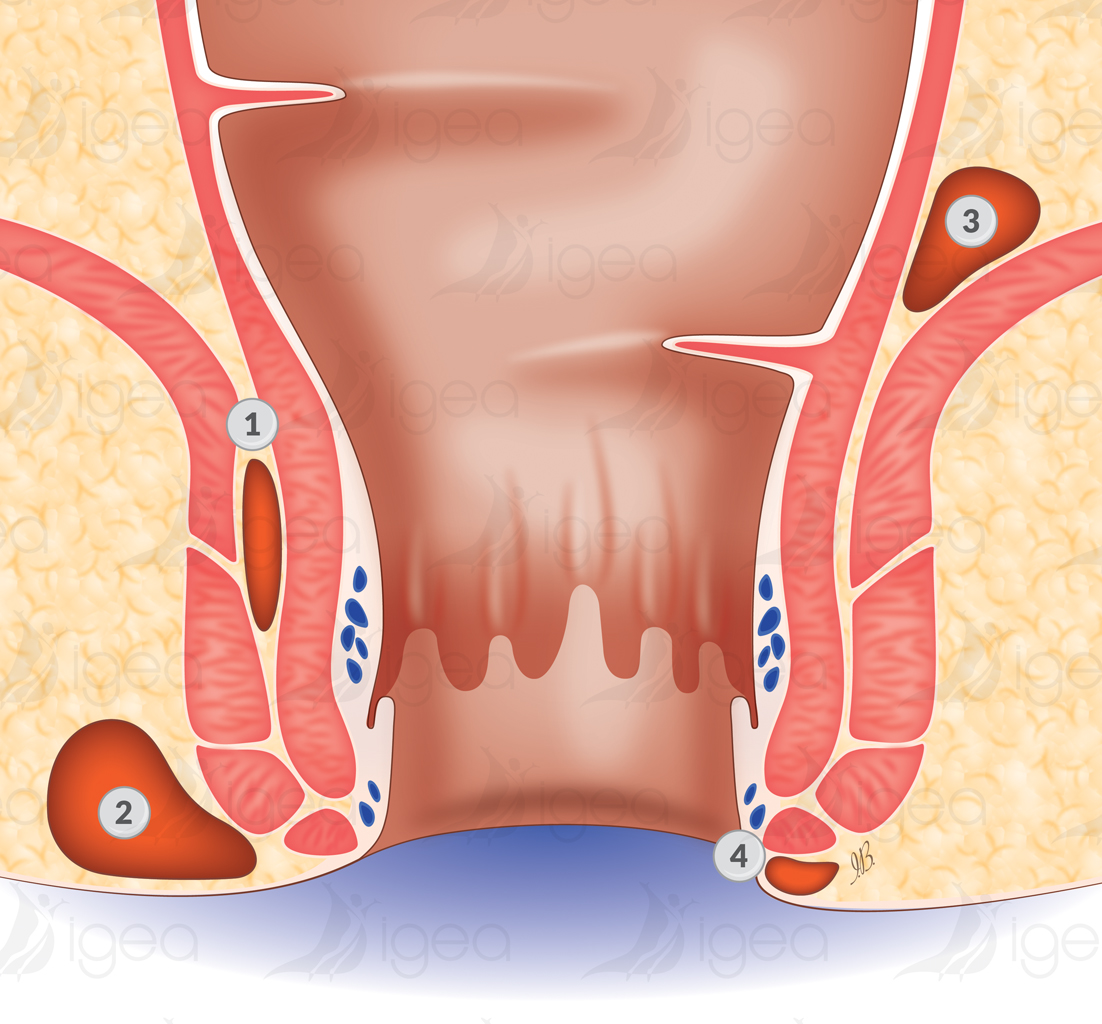
An anal abscess is a painful condition where a collection of pus develops around the anus.
The origin of the abscess is an infection of one of the glands normally present in the upper part of the anal canal, in the thickness of the sphincter muscle.
These glands have an opening towards the interior of the anal canal. They can become obstructed and infected by germs present in a bowel movement. The reasons why an anal gland becomes infected are not known.
Once a gland is infected an abscess forms very quickly.
The infection perforates the rectum wall and provokes the contamination of the surrounding fat.
A pocket filled with pus will expand under the skin around the anus, more or less rapidly.
Anal abscess:
An acute problem which anyone can have, without any particular cause. As many men as women, often between 30 and 50 years of age, but also children and old people.
There is no particular reason or cause as to why they appear. You may have only one such anal abscess during your lifetime, unless you suffer from Crohn’s disease which causes inflammation of the digestive tract.
Other abscesses, however, can form in the anal region, less frequently, and not related to an infected anal gland. They are predominantly related to skin diseases (Verneuil’s disease, Sebaceous cysts) or the infection of a pilonidal cyst.
Symptoms
- Pain
- Swelling
- Fever
- Difficulty urinating
- Constipation
Diagnosis:
A clinical examination of the anal region will find a red swelling which is hot, inflammatory, and visible on one of the edges of the anus.
When touched (palpation), the swelling is painful. It can seem hard, infiltrated or already changing if the abscess has become a localized collection of pus.
If the abscess is deep, the diagnosis is harder to make and can be confused with a tumour.
In this case, fever and hyperleukocytosis, however, will favour the hypothesis of an abscess.
Examination under general anaesthetic:
It is, in fact, the examination made under a general anaesthetic which confirms the diagnosis and provides more precision as to the seat and exact extent of the collection of pus.
Surgical Treatment
Opening the abscess and evacuating the puss is urgently required!
To reduce pain and avoid the infection getting worse, it is necessary to quickly open the abscess.
This is possible with a simple local anaesthetic but we prefer a general anaesthetic.
The patient is placed in the supine position, with legs bent (dorsal « frog-leg » position).
The operation involves making an incision in the abscess to evacuate all the infected tissue.
A finger is used to gently collapse the walls of the abscess to make sure that all tissue is evacuated.
The abscess is then washed with betadine (Povidone-iodine) and oxygenated water, and drained by using a wick or a corrugated rubber drain.
We always look for a communication with the infected gland (course of the fistula).
When such a communication is found, we must drain it and treat it.
If the draining of the abscess is executed correctly, antibiotics will not be necessary.
The use of anti-inflammatories should be avoided as they can aggravate the abscess.
Once open, the abscess will continue to empty itself for a few days, and will then close itself progressively.
Complete relief upon awakening.
The dressing is changed every day. Sometimes, antibiotics are prescribed for 5 days.
Paraffin oil and lactulose are given to the patient each morning to facilitate bowel movement. (Transulose, a French lubricating laxative medicine is prescribed at 1-3 teaspoons per day).
Local hygiene is very important. Preferably use a bidet/bath with warm water or wash with soft water.
Primary wound healing is completed after 10 to 15 days.
Complications
Recurrence:
It is difficult to tell whether or when an abscess may occur again: in a few weeks, months or years.
A fistula course exists, more or less directly, between the orifice of the infected gland in the anal canal (cryptitis) and the skin of the external orifice.
Anal fistula:
It is this fistula course (fistula also called anal fistula) that must be treated to avoid recurrence.
Fournier gangrene (acute necrotic infection/gangrene of the scrotum or perineum):
Certain abscesses are seriously infected at the outset and contain anaerobic bacteria.
These bacteria develop without needing oxygen, and produce toxins and gases.
In this case, which fortunately is exceptional, the infection spreads rapidly in the tissue around the anus, and can even spread to the genital organs, the stomach, and the totality of the buttocks.
Gangrene of the scrotum or perineum (Fournier gangrene) is a very serious medical condition.
Treatment:
- Early and regularly repeated surgical excisions under general anaesthetic.
- Use of a Vacuum Assisted Closure (VAC) dressing.
- Use of a suprapubic catheter.
- Putting in place a colostomy discharge bag.
Although a lot of care and energy is put into the treatment of this condition, there is still a high rate of mortality.
For fragile patients, for example those with diabetes, the development of the condition often leads to death, even if the treatment has been followed scrupulously.
The serious evolution of the condition to a sceptic shock (anaerobic gram-negative bacilli) can develop very quickly (in a few days), or at the outset, or from an abscess that has not been treated.
Riferimenti bibliografici
- Reference 1 : Test1
- Reference 2 : Test
- Reference 3 : Test
- Reference 4 : Test
- Reference 5 : Test
- Reference 6 : Test
- Reference 7 : Test
- Reference 8 : Test
- Reference 9 : Test