– – Cancer of Rectum – – Definition Colorectal Cancer
Cancer colorectal is the second cause of cancer and cancer death in Europe and touches the men as much as the women.
More than 35000 new cases are detected each year.
A tumour colorectale can be benign or malignant. A cancer with metastatic potential can be propagated with other parts of the body.
The cells of the mucous membrane of the colonist divide and reproduce in an ordered way. A cell can multiply without control and form a tumour.
Fortunately, cancer colorectal is avoidable and curable if it is detected early.
It is about a tumour for which we made to important progress these last 20 years, thanks to
- a better Prevention
- a better Tracking
- with progress of the Surgery (Resection of the Rectum by Laparoscopy with TME) and of
- Radio-Chemotherapy
- like with a better disciplinary assumption of responsibility multi.
– – Causes and Risk factors Cancer Colonist Rectum
Cancer colorectal begin with polyps (tumours of the wall of the colon). All the polyps do not become cancers of the colon.
The polyps known under the name of adenomata are the precursors of cancer colorectal.
The risk factors of the adenoma and the development of cancer all are not identified.
The food rich in greases and weak out of fibres, the increase in the age and the genetic anomalies are the most known risk factors.
Each one of us is at colorectal risk of cancer.
The majority of the people who develop a cancer colorectal do not present any known risk factor.
However, there exist diseases or antecedents associated at an increasing risk to develop a cancer colorectal:
- Chronic inflammatory diseases of the colon (ulcerous colitis or the disease of Crohn)
- Family or personal antecedents of cancer colorectal
- Adénomateux polyps
- Hereditary syndromes: polypose adénomateuse family; syndrome of Lynch – HNPCC
– – Symptoms of Cancer colorectal
Most people reached of cancer colorectal do not present any symptom.
The symptoms of cancer colorectal are often not very specific; it will be necessary to discuss it with your attending physician
- Changes in the practices of defecation with the appearance of a constipation alternated with a diarrhoea
- unexplained anaemia
traces of blood in the saddles (occult or obvious) responsible for the anaemia which involves a tiredness
- weight loss
- abdominal pains with type of intermittent intestinal colics with distension: they can last 1 to 2 days and be followed by a stinking diarrheal rout (syndrome of Koenig)
- feeling of “false needs”
- more rarely diagnoses it is made in urgency.
The symptoms are related to a revealing acute complication of the tumour with standard occlusion (the tumour blocks the transit completely) or perforation with peritonitis.
However, as we already said, most people, with polyps or a cancer of the colonist, do not present any symptom.
For this reason, it is very important to pass regularly from the examinations of tracking of cancer colorectal.
– – Preoperative Radiochimiotherapy
Operational pre Radiochimiothérapie
The radiotherapy is recommended into preoperative in all stages II and III (stages cT3, cT4 or N+) because it decreases the risk of repetition locorégional.
It makes it possible to reduce the size of the tumour by facilitating the preserving surgery and to decrease by 30 to 50% the risk of repetitions in small basin.
The Radiotherapy also applies to the ineradicable tumours from the start (fixed).
It is delivered over one 5 weeks duration in partnership with a chemotherapy known as concomitant to make it more effective.
The surgery is programmed 5-6 weeks later.
– – Surgical treatment of Cancer of Rectum
Surgical treatment of Cancer of Rectum

The radiotherapy and chemotherapy are sometimes used in complement and preparation of the Surgery
Cancer colorectal requires an intervention of resection (withdrawal of the tumour) in almost all the cases, for a complete cure.
The standardized surgical technique contributed to improve the rate of conservation of the anus (95%) and to reduce the rate of local repetition and the sexual surgical after-effects to turbid type of ejaculation and impotence.
The intervention consists in releasing the left colonist and removing the rectum with the tumour and the ganglia of vicinity. The released left colonist is used to restore (95% of the cases) digestive continuity by making an anastomosis colo – rectal without tension (joining of the left colonist on the rectum).
This technique is the former resection of the rectum with ablation of the mésorectum which we carry out principle by laparoscopy.
The mésorectum is a greasy fabric which surrounds the rectum and contains ganglia. It is delimited by a aponévrose, the fascia recti.
It is very clearly proven that the complete ablation of mésorectum (TME), with a fascia recti not broken decreases the risk of local relapse. The quality of the surgical gesture depends on the experiment of the surgeon in cancerology and laparoscopy.
Risk of Stomie after former resection of the rectum
Thanks to technical progress, less than 5% of all the operated patients of resection of cancer colorectal need an amputation abdomino-périnéale with installation of final colostomy.
When it is not possible to preserve the anal sphincter, the surgical gesture understands a exérèse of the rectum, anus and of sound sphincter (it is the amputation périnéale) and poses it of a final colostomy (intervention of Miles).
A stomy is the meeting of a segment of the intestine (colonist >> colostomy; iléon >> ileostomy) with the skin of the abdomen laterally to the umbilical point (left or on the right). The opening of the stomy constitutes the artificial anus.
It allows the collection in a pocket of the faeces of which the evacuation any more is not controlled by the sphincter of the natural anus.
The stomy associated with a resection with cancer with the rectum is temporary: it is generally about a ileostomy.
It will be then closed, after having checked by radiological control the good cicatrization of the digestive joining (opacifying without escapes on the level of anastomosis colorectale).
The closing of the stomy by local access is classically carried out 6 weeks after the resection of the rectum. An early closing with J 10, during the same hospitalization, is sometimes possible. Nevertheless, this stomy can be final if it is carried out within the framework of a cancer very low located and not allowing to save the sphincter (final colostomy associated with amputation of the rectum).
– – Complications Surgery of the Rectum
The surgery of the rectum can be burdened with an important morbidity.
The most dreaded complications are those which can oblige with the recovery with the surgical unit (D intervention):
- Leak which can involve peritonitis, pelvic abscess, delay of resumption of the /occlusion transit
- operational recovery with disassembling of the anastomosis or realization of stomy of discharge
- haemorrhage/bruise
- Unperceived wound of other bodies (bladder, ureter, urethra, small intestine)
- mechanical occlusion on support
- Urinary complications
- Sexual complications: Retrograde risk of ejaculation and impotence
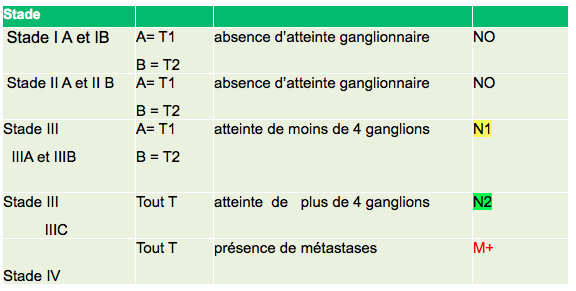
– – Stadification of Colorectal Cancer
Stadification of Colorectal Cancer
Once réséquée by surgical operation, the tumour is analyzed by the anatomopathologist.
It is classified compared to the size and the parietal depth of the attack (T), the invasion of the ganglia (NR),
the presence of remote localizations /m étastases (M).
Classification TNM allows ainside to define the stage of cancer colorectal (photographs)
Classification AJCCC
80 to 90% of the patients are cured if cancer is detected and treated in the first stages.
The rate of cure falls to 50% or less if the diagnosis is done at the later stages.
– – Auxiliary chemotherapy
Auxiliary chemotherapy
Chemotherapy (CT) postoperative (or auxiliary) is used when there are risks of repetition.
It is useful to eliminate the cancer cells which would have migrated towards other parts of the organization.
At a patient who received a preoperative radiochimiotherapie:
- If the ganglia are not invaded (tumour ypT1-3, N0 is stage I or II) a treatment of post-operative CT is useless (agreement of experts)
- In the event of ganglionic invasion (stage III is all Pt, N1-2) the abstention and the post-operative CT are the alternatives to be discussed according to factors of bad forecast: (ypT4, N2, engainement perish-highly-strung person, absence of total excision of the mésorectum)
– – Prevention
Prevention Colorectal Cancer
There exist measurements which reduce the risk to contract the disease.
The first consists in eliminating from the benign polyps by a coloscopy.
Besides eliminating the polyps, the long flexible tubular instrument used in this procedure envisages a thorough examination of the colon.
Although that is not proven, it seems that the food mode can play a significant role in the colorectal cancer prevention.
In so far as we know it, a high percentage of fibres, a mode low in greases are the only ones measures food which could help to prevent cancer colorectal.
Lastly, you must be vigilant on any change in your intestinal practices and ensure you that examinations of the colon are included in the medical examinations of routine once you are within the framework of the “high risk”.
Although the haemorrhoids cannot lead to the cancer of the colon, they can produce symptoms similar to those of the polyps of the colon or cancer. If you feel these symptoms, speak in to your attending physician.


Commentaires récents