The ascending colon or right colon
Definition
A cancer of the right colon is located on the right-hand part of the colon which goes from the caecum to the right colic angle.
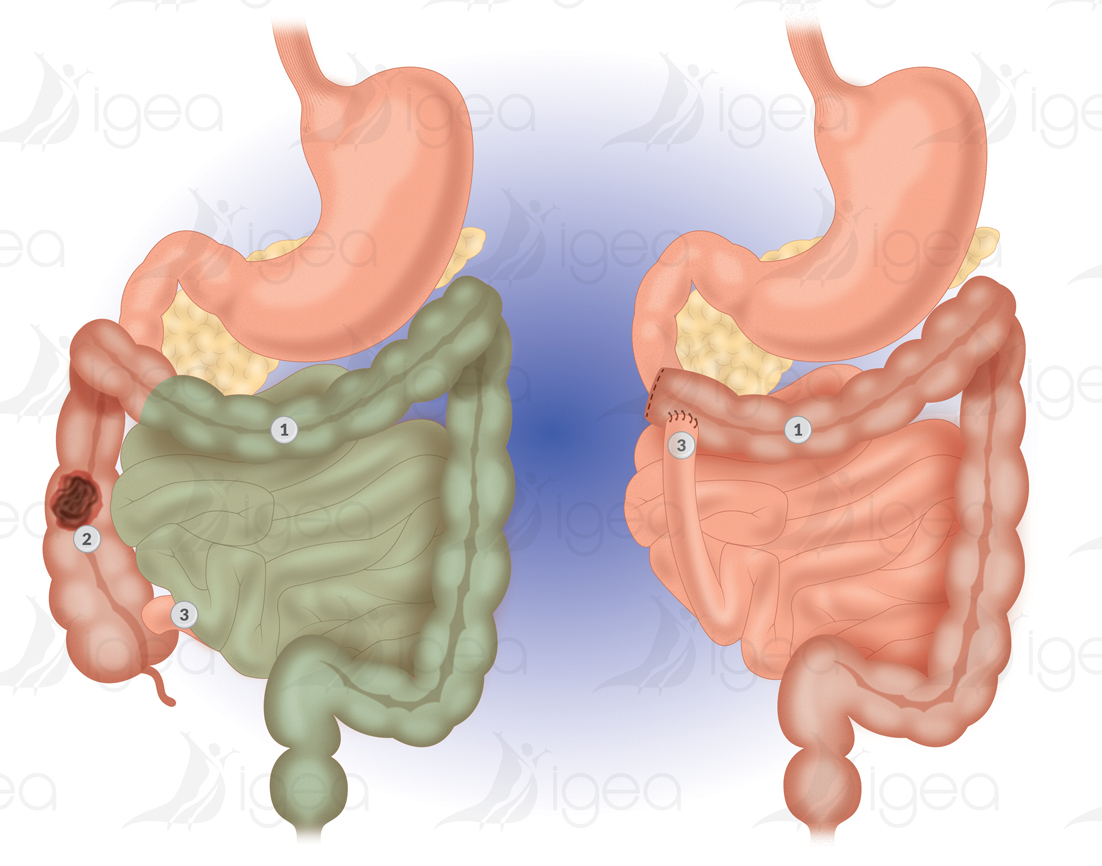
This surgical condition is treated by carrying out a right hemicolectomy.
This is a resection of the right colon, with re-establishment of digestive continuity.
This carried out with a suture (ileo transverse anastomosis) between the distal small intestine and the transverse colon.
Risk factors of a cancer of the right colon
- Polyps
Between 60 and 80 % of cancers of the colon develop on precancerous benign tumours: polyps or adenomas. The frequency of such lesions regularly increases with age. As shown by observations at autopsies, 12% of people under 55 have such a condition.
- Age
Rare before 40 years of age (cancer of the colon).
- Heredity
Globally, if a first-degree parent has a cancer, it multiplies by two the risk of contracting a cancer.
- Family Syndromes
Certain family illnesses carry a major risk of colon cancer. In particular familial adenomatous polyposis which is characterised by the early appearance of multiple polyps all over the colon, and the Lynch syndrome (also known as hereditary non-polyposis colorectal cancer – HNPCC).
The early development of a cancer is inevitable with familial polyposis.
With the Lynch syndrome the risk is extremely high, but comes a little later. It is associated with an increase in the frequency of endometrial cancers as well as, less frequently, other cancers (stomach, ovaries, urinary tract… )
- Inflammatory bowel disease
The influence of Crohn’s disease on cancer of the colon has remained controversial for a long time.
Ulcerative colitis is a classic risk factor for colorectal cancer. Howerer, the risk is a function of the extent to which the colon was affected over time.
Today, it is clear that this disease is also an important risk factor when it affects the whole colon, and if it started at a young age.
- Food
Other risk factors for colon cancer have been raised, such as a diet low in fibre and high in fats.
However, certain data suggests that the chronic use of nonsteroidal anti-inflammatory drugs may have a protective effect. But these factors remain very controversial.
Surgical Treatment
Right hemicolectomy
Operative indications:
- Cancer of the right colon: caecum, the ascending colon, right colic angle.
- Colic polyp unresectable by endoscopy.
- Crohn’s disease affects the ileum (terminal small intestine)
Cancer surgery involves the exeresis of the end of the last ileal loop and the colon up to the right third of the transverse.
An initial ligature must be made of the superior right colic vessels, then the middle colic vessels, and ileo-caeco-colic appendicular vessels in contact with the superior mesenteric artery.
Restoring continuity is made at the same time with anastomosis ileo-transverse termino-terminal or termino-lateral.
The surgery can be undertaken:
- Either by using a traditional technique,
- Or by laparoscopy/coelioscopy/keyhole surgery (mini invasive, with no large incision in the abdomen).
The surgical act takes longer with a laparoscopy than with traditional open surgery.
The renewal of bowel movements and food intake are probably more rapid after a right colectomy using laparoscopy.
The time spent in hospital is probably little different depending on the technique used.
There is no difference in the carcinological quality of the resection, or the quality of post-operative life, between a laparoscopy or traditional open surgery.
For Crohn’s disease, substantial parietal and aesthetic benefits exist in the long term use of laparoscopy (young patients and frequent surgery).
Complications after a Right hemicolectomy
- Complications are rare.
- It is surgery which is carried out regularly.
- The technique, either by laparoscopy, or by open surgery, is standardised, safe and reliable.
An anastomotic fistula is a major complication after a colon resection.
The risk of contracting a fistula is estimated at between 1% and 3%. It is a leakage of matter via the colon stitching, as the stitches are not hermetic.
This fistula may cause post-operative peritonitis, which requires urgent surgery and sometimes the creation of a double barrel stoma (artificial anus) with disassembly of the anastomosis.
Intestinal occlusion
Difficulty restarting bowel movement may make it necessary to undergo a scan to eliminate the diagnosis of a post-operative bowel obstruction with fibrous adhesions or an internal hernia (blocking of a loop of the small intestine in a gap created by the surgery)
Abscess of the abdominal wall is rare after laparoscopic surgery.
Other risks are inherent to all types of abdominal surgery:
- Damage/iatrogenic lesions of another abdominal organ.
- Haemorrhage.
Anticoagulants are prescribed to reduce the risk of thrombosis and/or pulmonary embolism.
Symptoms
A cancer of the right colon can develop over a long period of time without showing any signs or symptoms. When symptoms do appear, they are often vague, and can be confused with those of more common conditions. It is important to see a doctor.
Symptoms of a cancer of the right colon
- Melaena or rectal bleeding? Presence of blood on or in bowel movements (very dark colour of bright red).
- Fatigue linked to anaemia – usually after bleeding in the intestine.
- Loss of weight or an alteration of general state of health.
- Diarrhoea, constipation, or both alternately: unusual bowel movements (during a prolonged period).
- Indicative complications of a tumour of the right colon:
- Intestinal occlusion or perforation (infectious complication such as a paraneoplastic abscess)
- Metastatic liver
Pre-therapeutic Diagnosis and Assessment
The diagnosis of colon cancer is based on the colonoscopy which allows the tumour to be visualised, a tissue sample to be taken, and to look for any synchronous lesions (of the rectum and the left colon).
The pre-therapeutic assessment of a cancer of the right colon must include looking for visceral metastases with an hepatic ultrasound scan and eventually a thoracic-abdominal CT scan.
A carcinoembryonic antigen (CEA) test is useful to check the evolution after the treatment.
Important
Right colectomy
Surgery consultation Right Colectomy
- A meeting with the anaesthetists will be organised (please complete the medical questionnaire for our colleagues).
- A prescription will be given to you for ORAL IMPACT: which you should start to take 7 days before the surgery. This oral food supplement is a medicine which helps reduce post-operative complications, by increasing your immune defenses.
- In case you have a laparoscopy, you will receive a prescription for an abdominal immobilisation belt (please remember to bring it the day of your surgery).
- You will be given an informed consent form, to be completed, signed and returned before you are hospitalised.
- You will be given an estimate of any extra costs, to be sent to your private health insurance company (to obtain in advance their agreement to reimburse you).
- An invoice will be given to you when you leave, which you will need in order to be reimbursed by your private health insurance.
- You will be given a form to reserve your bedroom, whether single or double/shared. Single rooms are subject to availability.
The day before Right Colectomy surgery
You will be hospitalised in the clinic the day before the surgery, at around 4pm, with paramedical personnel taking care of you.
- You will need to go through the ADMISSIONS process for administration purposes, and afterwards you will be taken to the Service where you will be welcomed by a nurse.
- You must tell the nurse if, after your hospitalisation, you want to be transferred to a nursing home for convalescence, before returning home definitively.
- Don’t forget to check that the nurse has the telephone number of your support person, as the surgeons might need to contact them.
- Remember to give the nurse your Admissions File, the informed consent form, the blood test results, and morphological examination results, and the abdominal immobilisation belt in case you have a laparoscopy.
- Meeting with the Anaesthetists and Surgeons.
- Antiseptic shower (meeting with auxiliary nurse).
- Evening meal, then fasting from midnight prior to the general anaesthetic.
- If you are not having a pre-operative coloscopy, you will not need to clean out your bowel before surgery.
Colectomy surgery and your stay in the Clinic
Right Colectomy surgery lasts between 1h to 2-3 hours. The surgery takes place under a general anaesthetic.
You will be offered a spinal block anaesthesia: this is an anaesthetic injection directly into the spinal column. Spinal block anaesthesia reduces all post-operative pain.
It is often proposed for Right Colectomy surgery by laparoscopy.
During surgery, it will be administered by perfusion, by using either a central or a peripheral IV line.
Also a urinary catheter is passed through the urethra or a suprapubic catheter is inserted through a hole in the abdomen directly into the bladder (we prefer the latter for male patients).
- After the operation you will wake up in the Recovery Room. When ready, you will be transferred to the Surgery Department or the Surgery Intensive Care Unit.
- The Surgeon and the Anaesthetist will make the decision, if necessary, to transfer you to the Surgery Intensive Care Unit, where there is better surveillance, and any complications can be dealt with immediately. Your surveillance monitoring will cover your pulse, blood pressure, heart rate, temperature, diuresis, and an overview.
- Concerning information for a patient’s family, please note that the surgeon is available in the evening after the afternoon consultations.
- The evening after you have the surgery, you will continue to fast, take your anti-pain medicines whether intravenously and/or by spinal block anaesthesia.
During the following days, and with the agreement of the surgeon, you will be transferred either to a single room or a double/shared room.
Food intake will be progressive, and treatments will be given orally.
Prevention of thrombosis and gastric protection are systematic.
Leaving the Clinic after a right Colectomy
If you are returning home, you will leave the clinic at the end of the morning.
A hospitalisation report (+ an Operative report) is systematically sent to your GP/Family Doctor and all other correspondents (gastroenterologist, cancer specialist/oncologist, …).
- You will be given Prescriptions for painkillers and Low Molecular Weight Heparin (LMWH), in order to avoid any secondary thrombosis and pulmonary embolism.
- And a prescription for a home visiting nurse for the injections of Heparin and any localised care required.
- A doctor’s fit note will be provided if necessary.
- You will have the use of an abdominal immobilisation belt if you have surgery by laparoscopy.
- A future appointment with the surgeon will be made.
- We recommend that you walk a lot but avoid carrying heavy loads.
- When you get home you can take a shower, if you don’t have any localised care treatments at the level of the abdominal wall.
- You must wait for at least two weeks before bathing in soft water or in a swimming pool.
- As far as food is concerned, no special diets are required, but it is necessary to adapt your food intake relative to your bowel movements. For example:
- drink adequate amounts of water;
- if you are constipated eat more fruit and vegetables;
- and if you have diarrhoea, eat more pasta and rice.
- In fact, your bowel movements will be disrupted for 3 or 4 months.
- If you are transferred to a convalescent care home, your medical file will be immediately sent to the structure concerned.
- In any case, if you undergo cancer surgery, your file will be presented and discussed in a multidisciplinary meeting including surgeons, radiologists, gastroenterologists and cancer specialists/oncologists.
- Depending on the histological results of the surgical sample, you may be offered chemotherapy treatment.
Riferimenti bibliografici
- Reference 1 : Test1
- Reference 2 : Test
- Reference 3 : Test
- Reference 4 : Test
- Reference 5 : Test
- Reference 6 : Test
- Reference 7 : Test
- Reference 8 : Test
- Reference 9 : Test