Treatment for Anal Fistula
Definition
A fistula is an abnormal connection between two organs which normally have no such connection.
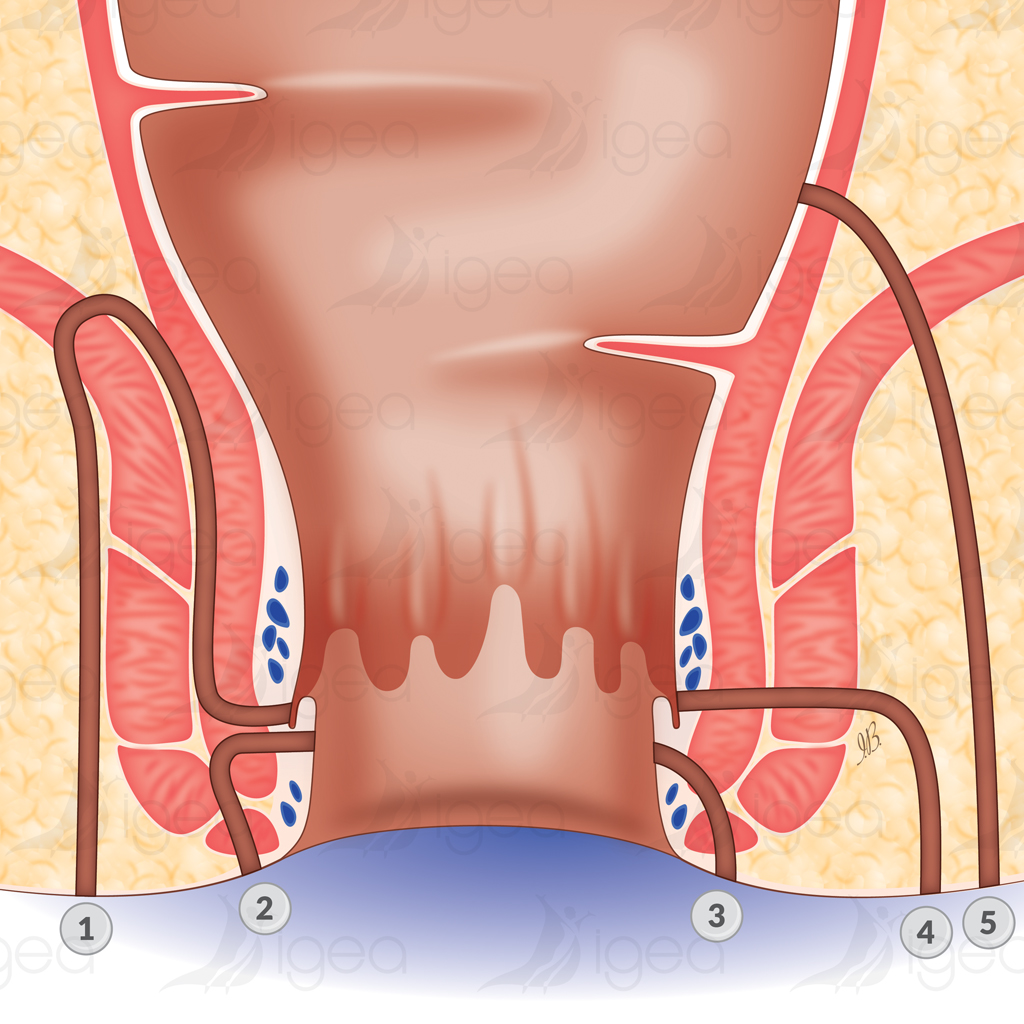
An anal fistula connects the interior of the anal canal and the skin near the anus. It is a sort of small tunnel which develops through the muscles of the anus (sphincters) and opens out on the skin by an orifice called an external orifice (or secondary orifice).
They are usually the result of an infection in small glands located inside the anus (glands of Hermann and Desfosses).
We do not know exactly why these glands become infected.
The anal fistula starts in the anal canal: called an internal orifice (or primary orifice).
The initial infection creates a small abscess located between the internal sphincter and the external sphincter.
From that starting point, the fistula can pass through the external sphincter at different heights.
Low transsphincteric fistula: if the fistula passes through the lower part of the muscle.
High transsphincteric fistula: if more than half of the muscle (or all of it) is involved.
Horseshoe fistula: where the trajectory passes to the opposite side by precise anatomic spaces.
In other cases, rather than passing through the external sphincter, the fistula moves upwards in the space located between the two muscles. This is called an intersphincteric or intramural abscess.
Clinical Manifestations
Two main forms exist: an acute form which is an abscess, and a chronic form with a simple discharge.
Acute form: abscess
The abscess creates localised pain in one part of the anus.
The intersphincteric (or intra-mural) abscess takes a particular form which creates pain high up in the rectum, without lumps at the level of the anal margin, and often creates urinary problems.
For this form of abscess, an examination is very painful, as it is necessary to evaluate the size of the abscess and eventually find the primary orifice The abscess, whether incised or which opens spontaneously, will develop into a chronic form with discharge, which will sometime cease and form a new abscess.
Chronic form: discharge
Can be present at the outset, or develop after the abscess had been incised, or can be a spontaneous evacuation.
The discharge can be more or less purulent and come from one or several orifices located in the skin of the anus: called an external orifice or a secondary orifice.
In the special case of the horseshoe fistula, there is an orifice on each side of the midline.
Complementary examinations are only useful with certain forms: particularly endo-anal ultrasound and an MRI scan can be requested with complicated forms or poly-operated forms.
Such examinations are made under a general anaesthetic, where the surgeon tries to determine the precise height of the course of the fistula and find the primary orifice responsible for the fistula.
Treatment
Anal fistulas connect the interior of the anus with the perianal skin.
Surgery has very satisfactory results: a recurrence rate of only 1 to 2 %.
1st principal of surgery: heal the fistula (or at least reduce the recurrence rate).
2nd principal of surgery: avoid anal incontinence.
At the abscess stage, the most important tasks are to reduce pain and evacuate pus by making an incision. Then the fistula can be treated.
The treatment for an anal fistula is actually surgical and complies with two imperatives: heal the fistula and preserve anal continence, as the muscles that ensure this continence are traversed by the fistula.
That is why, for certain forms, we will be obliged to proceed with a series of surgical interventions.
- Low fistulas:
- These require only one surgical act.
- The surgeon identifies the course of the fistula and the primary orifice by injecting a colourant into the internal orifice. The fistula is then removed right down to the muscle, which is simply severed.
- Post-operative care is simple, there is little or no pain.
- Such surgery can be carried out with a short stay in hospital of 48 hours, or as a day patient.
- Wound healing can take up to eight weeks.
- Complications are very rare (hypo-continence to flatus in around 1% of cases).
- Recurrence in centres used to this type of surgery is around 1%.
- High fistulas:
- Such fistulas are more rare and must be operated twice with a gap of roughly 2 months in between.
- With the first operation, the course of the fistula is removed right down to the muscle, a loose seton is placed in the space vacated (cotton or other absorbent material left with the ends protruding, to promote drainage of fluid or to act as a counterirritant).
- Post-operative care involves the wound being cleaned twice a day. The average stay in hospital is 2 to 3 days.
- We regularly check on the patient until the wound is completely healed, after which time we can consider undertaking the second operation, which involves, either a progressive section of the muscle by the seton which is tightened every 8-10 days, or by a direct incision.
- There are not many complications: exuding liquid in 2% of cases, hypo-continence to flatus, urgent need to go to the toilet when bowel movements are liquid in 11%. These problems reduce over time.
- Recurrence is around 2% in specialised services or those services used to this type of surgery.
- Particular cases:
- The horseshoe fistula sometimes requires three operations, the intramural fistula is open towards the interior of the rectum.
- Finally, certain particularly complex fistulas or poly-operated fistulas haven no systemic form of treatment.
Techniques of sphincter preservation:
It is always shocking to cut into a muscle which has an important function.
Which is why research is orientated towards muscle preservation in the treatment of anal fistulas.
The procedure of an advancement flap:
The course of the fistula is removed right down to the muscle and to the level of the rectum, a muco-muscular flap is used to cover the primary orifice.
The results currently available are discordant, so this technique requires further studies to be made.
The use of biological glue:
The ‘glue’ is injected into the course of the fistula to block it.
The results are still preliminary, but promising for simple fistulas.
Riferimenti bibliografici
- Reference 1 : Test1
- Reference 2 : Test
- Reference 3 : Test
- Reference 4 : Test
- Reference 5 : Test
- Reference 6 : Test
- Reference 7 : Test
- Reference 8 : Test
- Reference 9 : Test