Treatment for haemorrhoids

Definition and classification of haemorrhoidal disease
Definition and classification of haemorrhoidal disease
Haemorrhoids are veins, normally located in the rectum, or the anal canal.
The pathology and symptoms are linked to the swelling of these haemorrhoidal veins which increase in size and protrude from the anus.
The following types exist:
- An external haemorrhoidal network (external haemorrhoids), located under the skin of the orifice of the anus.
- An internal haemorrhoidal network (internal haemorrhoids), situated deeper and higher under the anal canal mucous membrane. It plays a role in the continence of the anus.
Haemorrhoidal disease is all of the troubles and symptoms which concern these vessels when they are swollen and irritated. These symptoms are generally benign and short-lived, but can generate discomfort in everyday life.
Haemorrhoidal disease is the source of various inconveniences: bleeding with bright red blood during or after bowel movement, pain around your anus, outbreak of oedematous skin (swelling of haemorrhoids), prolapsed haemorrhoid (a haemorrhoid that bulges outward from the anus), haemorrhoidal thrombosis (formation of a clot in a haemorrhoidal vein).
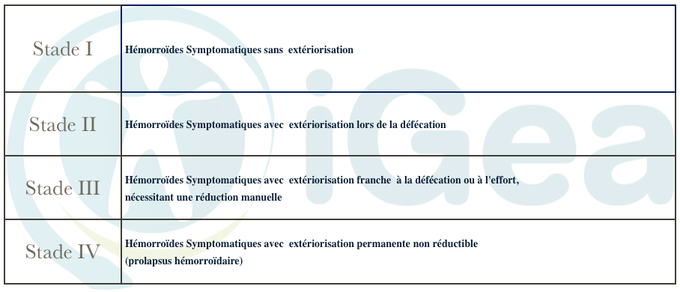
Haemorrhoid classifications
Caused by the effort of pushing too hard when having a bowel movement.
Haemorrhoids are divided into four stages, if they remain inside the anal canal (stage 1), where they permanently bulge outward from the anus (straightforward procidence stage 3 and prolapsed stage 4)
The type of treatment depends on the symptoms and stage of development (management of haemorrhoids disease: bibliography)
SURGICAL RECOMMENDATIONS
Surgery is recommended:
- When medical and medicinal treatments have failed (hygiene, diet, creams, ligatures) and symptoms reoccur or persist.
- Urgently for haemorrhoidal thrombosis.
- Or in the case of voluminous haemorrhoids (stages 3 and 4)
Classification in stages for Haemorrhoids disease:
Haemorrhoidal thrombosis
Around 15% of patients suffering from haemorrhoids will experience some form of thrombosis. It starts off as a small swelling, often just one, blueish in colour, hard under the skin at the edge of the anus. Then it naturally develops to a necrosis with the clot being evacuated, or where the clot is slowly absorbed ending up as a harmless anal skin tag growth (dermal after-effect).
The treatment for an external haemorrhoidal thrombosis, which is recent and painful, is to make an incision and extract the clot under local anaesthetic (an injection of lidocaine under and around the blood clot). An incision is made along the radial folds, followed by the excision from the rectal walls to avoid them closing prematurely.
The clot is removed and the cavity cleaned.
In the case of oedematous thrombosis, discovered late, or not very painful, the medical treatment is to use paracetamol along with non-steroidal anti-inflammatory drugs (NSAIDs) orally and the application of a cream containing corticosteroids.
Risk factors and Prevention of Haemorrhoids
Risk factors
Certains facteurs peuvent favoriser ou aggraver les symptômes de la pathologie hémorrhoidaire.
- Chronic constipation (effort used to expel bowel motions; staying a long time sitting on the toilet seat).
- Remaining standing/seated for a long time.
- Hereditary factors.
- Pregnancy, childbirth, premenstrual period (before menstruation).
- Excess weight and obesity.
- Certain sports and certain activities which involve lifting heavy weights.
- Drinking alcohol and eating spicy foods
Prevention of haemorrhoids
Combating constipation
- Vegetarian style diet, or diet rich in fibre (green vegetables and fruit).
- Staying well hydrated: drink 2 litres of water each day.
- Take regular physical exercise/sport.
Advice concerning bowel movements
- Try not to « hold back » from going to the toilet.
- Try not to stay too long on the toilet (don’t read when you are on the toilet) as this position encourages haemorrhoids to appear.
- Use a bidet/bath with warm water: 10cm of warm water in the bidet/bath (without adding foaming gel, bubble bath, soap or bath salts) to reduce swelling and calm anal pain/spasms.
Our advice
- Avoid coffee, beer, Coca-Cola, food which in too salty or too spicy.
- Avoid the temptation to scratch your rectum or anus if it burns or itches.
- It is recommended to use toilet paper which is not perfumed or coloured (less irritating).
SOS haemorrhoids Montpellier: Surgical treatment of haemorrhoids as an outpatient
The Management of surgery for haemorrhoidal disease takes place in our proctology unit, and prioritises the mini invasive approach (Medical literature: ‘Approach to haemorrhoids pub med’)
The techniques used in the IGEA centre for digestive surgery in Montpellier are: haemorrhoidectomy as per Milligan Morgan,
haemorrhoidopexy as per Longo,
and the painless mini-invasive method THD (transanal haemorrhoidal dearterialisation) with doppler guided artery ligation associated with a mucopexy (lifting and tightening of the anal canal).
We mainly use 3 different techniques which were evaluated in a retrospective study of 270 patients, published in 2019 by Dr SALSANO.
1 – Surgical treatment of haemorrhoids as an outpatient using the painless mini-invasive method THD (transanal haemorrhoidal dearterialisation) with doppler guided artery ligation associated with mucopexy
Painless mini-invasive method THD with doppler guided artery ligation associated with mucopexy.
The THD method surgery can be carried out on an outpatient basis (or 1 day surgery). The patient going home the same evening, with help at home from a paid carer (intravenous antalgic drip for 48 hours if necessary).
- The anaesthetist can carry out a pudendal nerve block procedure with an injection of local anaesthetic to temporarily reduce pain, and thereby reduce the need for further painkillers after the surgery.
- Haemorrhoidal tissue is not removed and the anatomy of the anal canal remains unaltered. This helps preserve those anatomic parts destined to control movements of the bowels.
- The surgical treatment is practically painless as there is no removal of tissue and the sutures are positioned above the jagged line, in an area without sensitive nerve endings.
- The patient can go back to work 10 days after the surgical treatment.
- Recurrence rate is very low.
- This procedure can be used for stage 2, 3 and 4 haemorrhoids, even with bleeding.
Please organise an appointment to discuss which is the best option for you.
2 – Haemorrhoidectomy using a modified version of the Milligan – Morgan technique
This classic procedure is the most complete and efficient technique to remove haemorrhoids.
It has been the most used operation for many decades, and generates few complications, giving the best results in both the short and long term.
The procedure consists of removing the haemorrhoid along with skin and mucous membrane, right up to the upper part of the anal canal.
Three excisions are made, corresponding to three haemorrhoidal bundles, between which
« bridges » of skin and mucous membrane are preserved. This helps the healing process and reduces the risk of infection and anal stenosis (abnormal narrowing).
3 – Haemorrhoidopexy as per Longo
This procedure, is a haemorrhoidectomy using stapling, which blocks blood circulation in the haemorrhoidal tissue. The stapling generally involves less pain than a classic haemorrhoidectomy, and allows the patient to go back to work earlier.
However, in comparison with the Milligan Morgan haemorrhoidectomy, stapling as per Longo is associated with a higher risk of recurrence and rectal prolapse.
THD, a painless method for treating haemorrhoids
This innovative and painless method allows a rapid return to normal activities for a frequent pathology whose treatment has always been considered to be painful and disabling.
The procedure involves a single-use, sterile surgical device which comprises an anuscope with sliding operating window (allowing the passage of the needle holder), a single-use Doppler probe, and a fibre optic lighting system.
The THD treatment is based on 2 concepts: 1) dearterialisation and 2) mucopexy or lifting and tightening.
1 – Dearterialisation / REDUCTION OF ARTERIAL PRESSURE IN THE ANAL CANAL
- Identification and selective ligation of 6 terminal branches of the superior rectal artery. These 6 branches are recognised using Doppler echography and then connected by absorbable sutures.
- Dearterialisation decongestion of haemorrhoidal bundles and correcting any bleeding.
2 – Mucopexy or lifting and tightening the anal canal / REDUCTION OF THE PROLAPSE BY LIFTING AND TIGHTENING THE ANAL CANAL
- The points of dearterialisation serve to fix a plication of the prolapse using overlock suturing. This allows the haemorrhoidal bundles to be replaced in their anatomical positions.
Benefits of THD
- Mini invasive and not traumatic.
- Can be carried out on an outpatient basis.
- Marginal postoperative pain.
- Rapid recovery.
- Extended indications.
- No serious complications.
Watch this surgery on Youtube
You need to be over 18 to watch this video. You must be connected to your Youtube account.
Postoperative follow-up
Postoperative follow-up after a haemorrhoidectomy or a haemorrhoidopexy
We monitor: postoperative pain, the return of urination, postoperative bleeding, the return of bowel movement.
Pain after a haemorrhoidectomy or a haemorrhoidopexy
- To reduce postoperative pain after a haemorrhoidectomy with our technique we use either ultrasonic or bipolar scissors.
- Analgesic/anti-inflammatory treatment is systematically administered during the first days after surgery.
- Pain will occur again with the first bowel movement after a haemorrhoidectomy.
- This treatment is completed by the prescription of the strong pain killer Tramadol or another derivative of morphine, by oral administration or subcutaneously.
Normal urination after a haemorrhoidectomy or a haemorrhoidopexy
We will ask you to urinate before the surgery takes place.
- It is important to be aware of the risks of a full bladder by favouring a general anaesthetic rather than spinal anaesthesia.
- The retention of urine is a source of pain which is sometimes difficult to specify.
- For a man, the administration of an antispasmodic and alpha 1 blocker agents must be considered before urinary catheterisation.
- A simple urinary catheter is all that is required for women.
Bleeding after a haemorrhoidectomy or a haemorrhoidopexy
- Light bleeding during the first bowel movement is frequent and nothing to worry about.
- Bleeding with the emission of blood clots may take place during the first hours or days, regardless of the surgical technique used, and mainly during the first two weeks.
- In case of bleeding, local packing is sufficient.
- In less than 3% of cases, new surgery is required urgently to carry out a haemostasis procedure under a general anaesthetic.
First Bowel Movement after a haemorrhoidectomy or a haemorrhoidopexy
- Laxatives are systematically prescribed after the operation in order to obtain an initial, soft bowel movement within 48 to 72 hours.
- In the case of a haemorrhoidectomy, it is advised to take painkillers before the first bowel movement, and not lock yourself in the toilet (due to the risk of vasovagal fainting).
Following bowel movements will be progressively less painful if you drink a lot of water and continue with the laxatives in order to obtain soft bowel movements.
- Pain will often disappear after the 10th day of convalescence.
Complications
Postoperative complications after treatment for haemorrhoids
Complications after a haemorrhoidectomy as per Milligan Morgan, or a haemorrhoidopexy as per Longo, are not very frequent.
There are 4 possible complications, but they are rare: post-operative bleeding, abscess, anal stenosis, recurrence of haemorrhoids.
Postoperative bleeding after surgical treatment for haemorrhoids
- Bleeding may occur during the first hours after surgery and may require surgical haemostasis treatment (2% of cases).
- Bleeding may also occur when a healing scab falls off (around the 10th day after surgery). The patient should immediately consult their doctor/surgeon for a decision whether or not surgical haemostasis treatment is necessary.
- To forestall this risk we use ultrasonic scissors (with an extra cost being added to the normal cost of the operation) and bipolar scissors.
Postoperative abscess after treatment for haemorrhoids
- Infection of the region operated is very rare.
- We systematically treat with antibiotics during the surgery, and after the surgery for 48 hours.
Postoperative anal stenosis after treatment for haemorrhoids
- Stenosis (narrowing) of the anal canal, is reported in case studies in 4% of cases.
- It is the exception if post-operative care is carried out correctly.
- This type of stenosis is uncomfortable, embarrassing and difficult to treat. It must be regularly monitored by the patient, making, as soon as possible, a daily rectal examination using a Vaseline covered finger cot (cover), until the post-operative consultation with the surgeon (after one month).
- If such a rectal examination is impossible due to the pain caused, the patient should contact the surgeon for a surgical dilation to be made, under a short general anaesthetic.
Recurrence of haemorrhoids
- Recurrence affects less than 1% of patients.
- With only one surgical operation it is impossible to remove, in totality, all very large circumferential haemorrhoids.
- For these reasons, only the largest haemorrhoids are resected.
- The definitive result will be judged after 3-4 months, as will any indication of a required further, complementary resection.
Riferimenti bibliografici
- Reference 1 : Test1
- Reference 2 : Test
- Reference 3 : Test
- Reference 4 : Test
- Reference 5 : Test
- Reference 6 : Test
- Reference 7 : Test
- Reference 8 : Test
- Reference 9 : Test